在我国肺癌的发病率和病死率在各种恶性肿瘤中位居首位[1],小细胞肺癌的恶性程度明显高于其他肺癌,预后差,未经治疗的小细胞肺癌中位生存期为2~4个月,2年生存率低于1%。早在19世纪Virchow就提出肿瘤可能源自慢性炎症,后来的研究也证实了这一观点[2],并提出了肿瘤微环境[3]。国外及国内均有研究证实中性粒细胞淋巴细胞比值(neutrophil lymphocyte ratio,NLR)与多种肿瘤的预后相关,如非小细胞肺癌、胃癌、肝癌、头颈部肿瘤、乳腺癌等[4-8]。目前关于NLR与小细胞肺癌预后关系的研究较少。本研究回顾性分析162例初诊未经治疗小细胞肺癌患者的临床资料,旨在探讨初诊时NLR与小细胞肺癌临床各因素及预后的关系。
1 资 料 与 方 法
1.1一般资料 选择华北理工大学附属医院2006年12月—2016年6月经组织病理学或细胞学首次确诊的小细胞肺癌患者162。其中男性122例(75.31%),女性40例(24.69%);年龄24~83岁,中位数年龄58岁,≥60岁70例(43.21%),<60岁92例(56.79%);吸烟者107例(66.05%),不吸烟者55例(33.95%);局限期75例(46.30%),广泛期87例(53.70%);ECOG评分0~1分组140例(86.42%),≥2分组22例(13.58%);放疗134例(82.72%),未放疗28例(17.28%);对初次化疗反应:完全缓解(complete remission,CR)8例(4.94%),部分缓解(partial remission,PR)125例(77.16%),疾病稳定(stable disease,SD)15例(9.26%),疾病进展(progressive disease,PD)14例(8.64%),化疗有效组(CR+PR)133例(82.10%),化疗无效组(SD+PD)29例(17.90%)。收集年龄、性别、吸烟史、肿瘤分期、ECOG评分、化疗方案、无进展生存期(progression free survival,PFS)、总生存期(overall survival,OS)、初诊时全血细胞计数等指标。通过病例检索及电话联系进行随访,随访日期截至2016年8月31日。
1.2方法 根据收集的临床资料建立EXCEL数据库,应用SPSS 22.0统计学软件进行分析。应用ROC曲线确定初诊时NLR最佳分界值。应用χ2检验分析各组临床特征与NLR之间的关系。应用Kaplan-Meier方法绘制患者生存曲线图;应用Log Rank进行非参数检验,分别分析高、低NLR组临床特征及其对小细胞肺癌患者预后的影响,不同组间采用χ2检验,得出影响小细胞肺癌PFS和OS的单因素。应用Cox比例风险回归模型进行多因素生存分析。P<0.05为差异有统计学意义。
2 结 果
2.1临床特征与NLR的关系 高NLR组男性明显高于女性,但所占比例与低NLR组男性所占比例差异无统计学意义(P>0.05);高NLR组ECOG评分≥2分的患者所占比例明显高于低NLR组,差异有统计学意义(P<0.05)。见表1。
2.2单因素分析临床特征与PFS、OS之间的关系 PFS 在患者NLR、肿瘤分期、有无放疗、化疗疗效之间差异有统计学意义(P<0.05),提示初诊时低NLR组、局限期、放疗且化疗有效的患者有较好的PFS,反之则差。OS在患者NLR、年龄、性别、肿瘤分期、有无放疗、化疗疗效之间差异有统计学意义(P<0.05),提示初诊时低NLR组、年龄低于60岁、女性、局限期、放疗且化疗有效的患者OS较长,反之则短。见表2。
表1 临床特征与NLR的关系
Table1The relationship between clinical characteristics and NLR(例数,%)
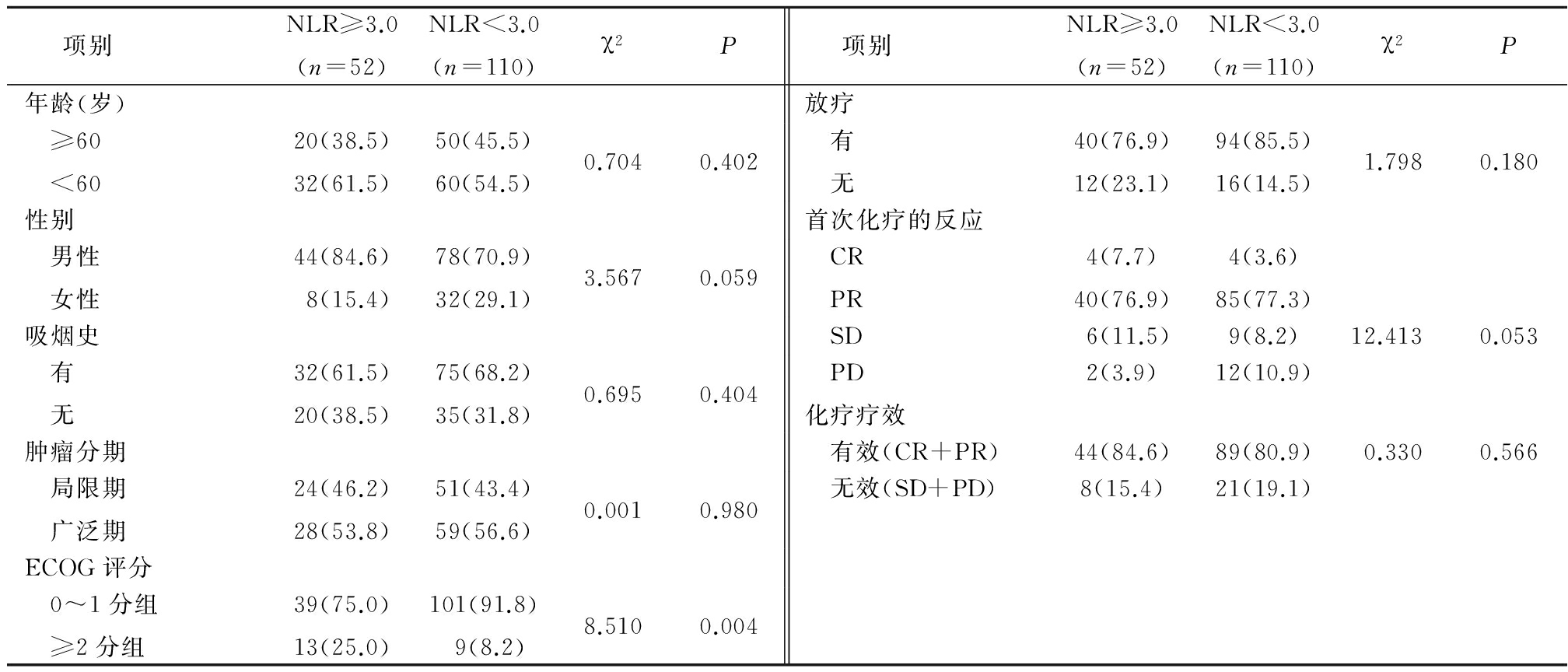
表2 临床特征与小细胞肺癌患者生存期的关系
Table2Relationship between clinical characteristics and survival of small cell lung cancer patients

2.3初诊时NLR与小细胞肺癌患者PFS、OS的关系 高NLR组和低NLR组中位PFS分别为6.0个月和7.5个月,差异有统计学意义(P<0.05),提示高NLR组PFS较低NLR组短;2组中位OS分别为10.7个月和14.3个月,差异有统计学意义(P<0.05),提示高NLR组OS较低NLR组短。以PFS、OS为横坐标,以累计存活率为纵坐标,绘制PFS、OS生存曲线(图1,2),通过分析PFS和OS生存曲线特征可以看出,同一时间截点处高NLR组累积生存率低于低NLR组。
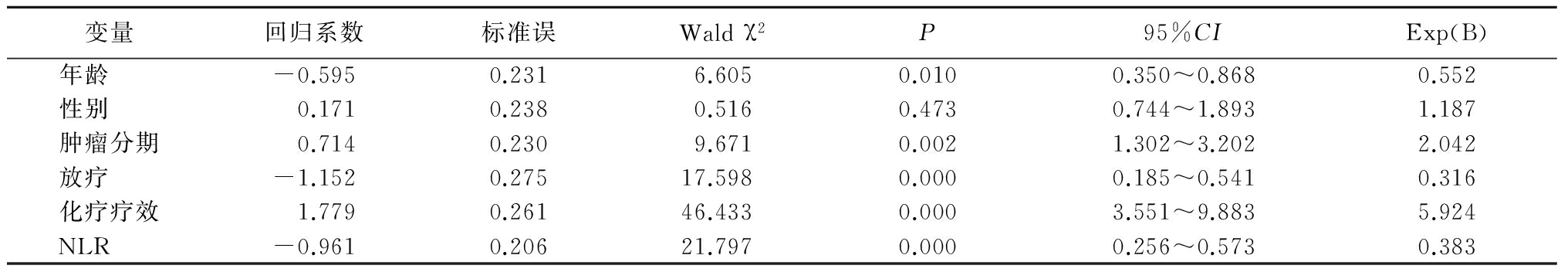
2.4多因素Cox回归模型分析临床特征与PFS、OS之间的关系 将对小细胞肺癌患者PFS和OS有意义的单因素分别作为自变量进行分析,得出化疗疗效为PFS的独立风险因素,年龄、肿瘤分期、放疗、化疗疗效、NLR为OS的独立风险因素(P<0.05)。见表3~5。
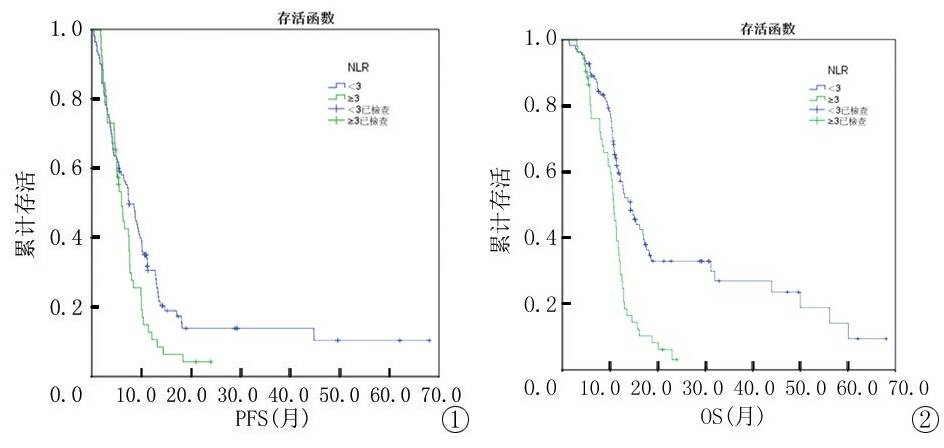
图1 NLR与小细胞肺癌患者PFS的关系图
Figure1Relationship between NLR and PFS of small cell lung cancer patients
图2 NLR与小细胞肺癌患者OS的关系图
Figure2Relationship between NLR and OS of small cell lung cancer patients
表3 变量赋值表
Table3Variable assignment table

表4 PFS多因素Cox回归分析
Table4Multivariate Cox regression analysis of PFS
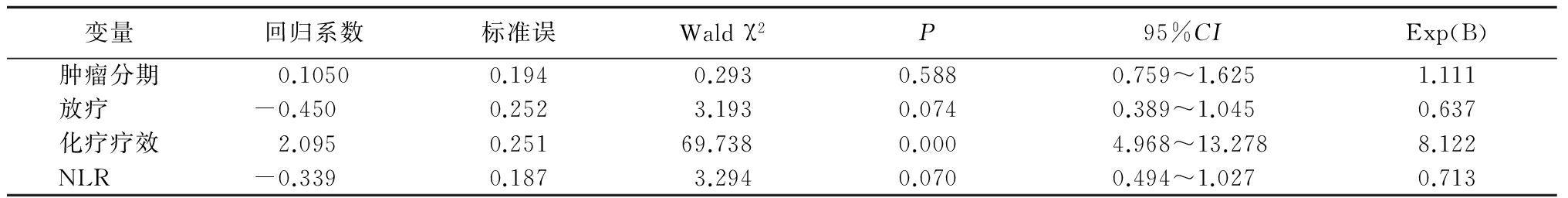
表5 OS多因素Cox回归分析
Table5Multivariate Cox regression analysis of OS
3 讨 论
肺癌按组织病理学可分为小细胞肺癌及非小细胞肺癌,小细胞肺癌是分化最低、恶性程度最高、转移早的肺癌类型[9]。在治疗方面小细胞肺癌仍以化疗和放疗为主,只有2%~5%的局限期患者可行手术治疗。虽然小细胞肺癌对化疗和放疗高度敏感,但易复发,与非小细胞肺癌相比,小细胞肺癌预后更差,经放化疗后5年生存率低于7%[10]。因此,找到能预测小细胞肺癌的预后因素尤为重要。癌症的预后与多种因素相关,炎性细胞与肿瘤的关系已成为被关注的热点[11]。多项研究表明,当肿瘤组织中有大量的中性粒细胞时,提示患者的预后不良[12-13]。淋巴细胞参与免疫应答,局部免疫效应作用越强,越不利于肿瘤生长转移,反之局部免疫抑制作用越强,越有利于肿瘤侵袭转移[14]。本研究得出相似的结果,当中性粒细胞数增多和或淋巴细胞减少均可导致NLR升高,NLR水平升高提示肿瘤患者预后不良。
本研究显示初诊时患者NLR水平与患者总体生存时间呈负相关,多因素分析显示NLR是小细胞肺癌预后的独立风险因素。这与Kang等[15]的研究结果一致。Azab等[16]对1 345例乳腺癌患者的 NLR 分析结果表明,NLR水平>3.3时患者1年及5年病死率分别为16%及44%,而 NLR水平<1.8时1年及5年的病死率分别为0及13%,从而认为 NLR是乳腺癌患者短期及长期病死率的预测指标。Forget等[17]分析了357例早期乳腺癌患者的NLR,结果显示乳腺癌患者NLR水平3~4时与高复发危险和高病死率相关。高NLR水平与癌症患者总生存期呈负相关。
本研究存在一定的局限性,符合纳入要求的样本量较少,随访时间长,难免存在偏倚,研究得出的结论应该在扩大样本量后进一步验证。如果能够得到更全面更系统的资料,可以更进一步进行多因素分析,从而能深化NLR与小细胞肺癌预后问题的研究。本研究显示初诊小细胞肺癌患者NLR水平与患者总生存期呈负相关,故NLR可作为评估小细胞肺癌预后的临床指标。
[参考文献]
[1] 陈万青,郑荣寿,曾红梅,等.2011年中国恶性肿瘤发病和死亡分析[J].中国肿瘤,2015,24(1):1-10.
[2] Zhang M,Zhou S,Zhang L,et al. Role of cancer-related inflammation in esophageal cancer[J]. Crit Rev Eukaryot Gene Expr,2013,23(1):27-35.
[3] 高广周,张泽,郝英霞.肿瘤间隙液的研究进展[J].河北医科大学学报,2015,36(11):1359-1362.
[4] Takahashi Y,Horio H,Hato T,et al. Prognostic Significance of Preoperative neutrophil-lymphocyte ratios in patients with stage Ⅰ non-small cell lung cancer after complete resection[J]. Ann Surg Oncol,2015,22(Suppl 3):S1324-1331.
[5] Yu L,Lv CY,Yuan AH,et al. Significance of the preoperative neutrophil-to-lymphocyte ratio in the prognosis of patients with gastric cancer[J]. World J Gastroentero,2015,21(20):6280-6286.
[6] Chen TM,Lin CC,Huang PT,et al. Neutrophil-to-lymphocyte ratio associated with mortality in early hepatocellular carcinoma patients after radiofrequency ablation[J]. J Gastroenterol Hepatol,2012,27(3):553-561.
[7] Haddad CR,Guo L,Clarke S,et al. Neutrophil-to-lymphocyte ratio in head and neck cancer[J]. J Med Imaging Radiat Oncol,2015,59(4):514-519.
[8] Azab B,Shah N,Radbel J,et al. Pretreatment neutrophil/lymphocyte ratio is superior to platelet/lymphocyte ratio as a predictor of long-term mortality in breast cancer patients[J]. Med Oncol,2013,30(1):432.
[9] Spigel DR,Socinski MA. Rationale for chemotherapy,immunotherapy,and checkpoint blockade in SCLC:beyond traditional treatment approaches[J]. J Thorac Oncol,2013,8(5):587-598.
[10] Bunn PA Jr,Minna JD,Augustyn A,et al. Small Cell Lung Cancer:Can recent advances in biology and molecular biology be translated into improved outcomes[J]. J Thorac Oncol,2016,11(4):453-474.
[11] Zhu Z,Shen Z,Xu C. Inflammatory pathways as promising targets to increase chemotherapy response in bladder cancer[J]. Mediators Inflamm,2012,2012:528690.
[12] Li QQ,Lu ZH,Yang L,et al. Neutrophil count and the inflammation-based glasgow prognostic score predict survival in patients with advanced gastric cancer receiving first-line chemotherapy[J]. Asian Pac J Cancer Prev,2014,15(2):945-950.
[13] Zhao JJ,Pan K,Wang W,et al. The prognostic value of tumor-infiltrating neutrophils in gastric adenocarcinomaafter resection[J]. PLoS One,2012,7(3):e33655.
[14] Pauken KE,Wherry EJ. Overcoming T cell exhaustion in infection and cancer[J]. Trends Immunol,2015,36(4):265-276.
[15] Kang MH,Go SI,Song HN,et al. The prognostic impact of the neutrophil-to-lymphocyte ratio in patients with small-cell lung cancer[J]. Br J Cancer,2014,111(3):452-460.
[16] Azab B,Bhatt VR,Phookan J,et al. Usefulness of the neutrophi tolymphocyte ratio in predicting short and long-term mortality in breast cancer patients[J]. Ann Surg Oncol,2012,19(1):217-224.
[17] Forget P,Machiels JP,Coulie PG,et al. Neutrophil lymphocyte ratio and intraoperative use of ketorolac or diclofenac are prognostic factors in different cohorts of patients undergoing breast,lung,and kidney cancer surgery[J]. Ann Surg Oncol,2013,20(Suppl 3):S650-660.