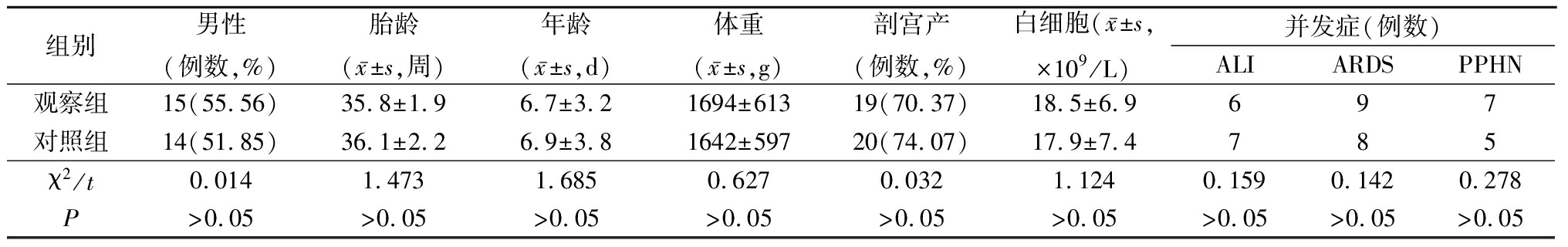
表1 2组一般资料比较
Table1Comparison of general data between two groups(n=27)
·论 著·
杨 丽,陈燕华,徐凤玲*
(江苏省泰州市人民医院儿科,江苏 泰州 225300)
[摘要] 目的探讨吸入一氧化氮(nitric oxide,NO)联合高频震荡通气(high-frequency oscillatory ventilation,HFOV)治疗新生儿重症肺炎的临床效果。方法选择 2012 年 1 月—2016年12月我院儿科收治的54例新生儿重症肺炎患儿作为研究对象,随机分为观察组(吸入NO联合HFOV治疗)和对照组(HFOV治疗),每组27例,分别记录2组治疗前和治疗后1,6,24 h呼吸功能指标和血气指标,以及治疗后肺功能指标和重度肺炎相关临床体征消失时间。结果2组平均气道压(mean airway pressure,MAP)、吸入氧浓度(fraction of inspiration O2,FiO2)、氧合指数(oxygenation index,OI)及动脉肺泡氧分压比值(a/A)在时点间、组间·时点间交互作用差异均有统计学意义(P<0.05),在组间差异无统计学意义(P>0.05)。2组动脉血氧分压(partial pressure of oxygen,PaO2)、二氧化碳分压(partial pressure of carbon dioxide,PaCO2)及pH值在时点间、组间·时点间交互作用差异均有统计学意义(P<0.05),在组间差异无统计学意义(P>0.05)。观察组治疗后用力肺活量(forced vital capacity,FVC)、1秒用力呼气容积(forced expiratory volume in one second,FEV1)、最大用力呼气峰流量(peak expiratory flow,PEF)明显低于对照组,差异均有统计学意义(P<0.05)。观察组治疗后重度肺炎相关的三凹征、肺部啰音、发热、发绀及鼻翼扇动等临床体征消失时间明显短于对照组,差异均有统计学意义(P<0.05)。结论吸入NO联合高频震荡通气治疗新生儿重症肺炎,可以明显改善患儿的呼吸功能和血气指标,并显著改善肺功能和重度肺炎相关的临床体征,具有一定临床应用和研究价值。
[关键词]肺炎;一氧化氮;胸壁震荡通气;婴儿,新生 doi:10.3969/j.issn.1007-3205.2018.09.011
新生儿肺炎是新生儿期最常见的疾病之一,可发生在宫内、分娩过程中及出生后,引发不同程度的缺氧和感染中毒症状[1],特别是重症肺炎患儿易发生急性肺损伤(acute lung injury,ALI)、急性呼吸窘迫综合征(acute respiratory distress syndrome,ARDS)和持续性肺动脉高压(persistent pulmonary hypertension,PPHN)等严重并发症,甚至死亡[2-3]。流行病学调查显示新生儿重症肺炎的发生率呈上升趋势[4]。近年来,吸入一氧化氮(nitric oxide,NO)疗法是治疗新生儿危重呼吸类疾病的临床研究热点[5],其主要作用机制是选择性舒张肺小血管平滑肌,降低肺循环阻力,不影响体循环血流动力学,有利于改善预后[6]。此外,机械通气策略也是一种治疗该类疾病的重要手段,包括常频机械通气(conventional mechanical ventilation,CMV)和高频震荡通气(high-frequency oscillatory ventilation,HFOV),其主要是通过提高肺氧合和改善肺损伤,以减缓呼吸衰竭进展[7]。然而,目前国内关于吸入NO联合HFOV治疗新生儿重症肺炎临床效果的报道较少。本研究旨在比较吸入NO联合HFOV治疗与单独应用HFOV治疗新生儿重症肺炎的临床效果,报告如下。
1.1一般资料 选择 2012 年1月—2016年12月我院儿科收治的新生儿重症肺炎患儿54例作为研究对象。纳入标准:①胎龄35~41周;②符合《实用新生儿科学》第4版中关于新生儿重症肺炎的临床诊断标准[8];③患儿家属同意并签署临床研究知情同意书。排除标准:①严重的先天性心脏病;②其他严重的遗传性疾病;③可能会影响研究结果的其他疾病。将所有患儿随机分为观察组(吸入NO联合HFOV治疗)和对照组(HFOV治疗),每组27例。2组性别、胎龄、年龄、体重、分娩方式、白细胞数目及并发症等差异均无统计学意义(P>0.05),具有可比性,见表1。
表1 2组一般资料比较
Table1Comparison of general data between two groups(n=27)
1.2治疗方法 患儿均先进行CMV治疗,采用同步间歇指令通气模式,当治疗无效或效果欠佳时,转为HFOV或吸入NO联合HFOV治疗,同时继续给予常规基础治疗,包括保持体温、营养支持、维持体内水电解质平衡、应用抗炎及心血管活性药物等。
1.2.1对照组 采用HFOV治疗,应用德国Stephnie公司生产的3100 型高频震荡呼吸机,设置机械通气参数以维持经皮血氧饱和度(percutaneous oxygen saturation,SpO2)≥90%,吸入氧浓度(fraction of inspiration O2,FiO2)≤60%。参数范围:震荡频率9~15 Hz,震荡压力幅度以胸部有较明显的振动为标准,平均气道压(mean airway pressure,MAP)高出CMV的2~4 cmH2O。
1.2.2观察组 采用吸入NO联合HFOV治疗, 在对照组HFOV治疗基础上接入NO(上海诺芬生物技术有限公司),初始浓度设置为20 ppm,观察20~30 min,若无效则将NO浓度上调5~10 ppm,达到40 ppm仍无效者停止吸入NO;若有效则连续吸入6 h后,将NO浓度每隔30 min下调 5~10 ppm 直至6 ppm, 维持吸入 NO 36~72 h。当氧合指数(oxygenation index,OI)<10 mmHg,动脉血氧分压(partial pressure of oxygen,PaO2)>60 mmHg, SpO2>90%,FiO2<50%时,停止吸入NO。应用加拿大PULMONOX H型NO 监测仪对 NO 的浓度进行监测。
1.3评价指标 ①2组治疗前和治疗后1,6,24 h呼吸功能指标,包括MAP、FiO2、OI及动脉肺泡氧分压比值(a/A);②2组治疗前和治疗后1,6,24 h血气指标,包括PaO2、二氧化碳分压(partial pressure of carbon dioxide,PaCO2)及pH值;③2组治疗后肺功能指标,包括用力肺活量(forced vital capacity,FVC)、1秒用力呼气容积(forced expiratory volume in one second,FEV1)及最大用力呼气峰流量(peak expiratory flow,PEF);④2组治疗后重度肺炎相关临床体征(包括三凹征、肺部啰音、发热、发绀及鼻翼扇动等)消失时间。
1.4统计学方法 应用SPSS 18.0 统计软件分析数据。计量资料比较分别采用两独立样本的t检验和重复测量的方差分析;计数资料比较采用χ2检验。P<0.05为差异有统计学意义。
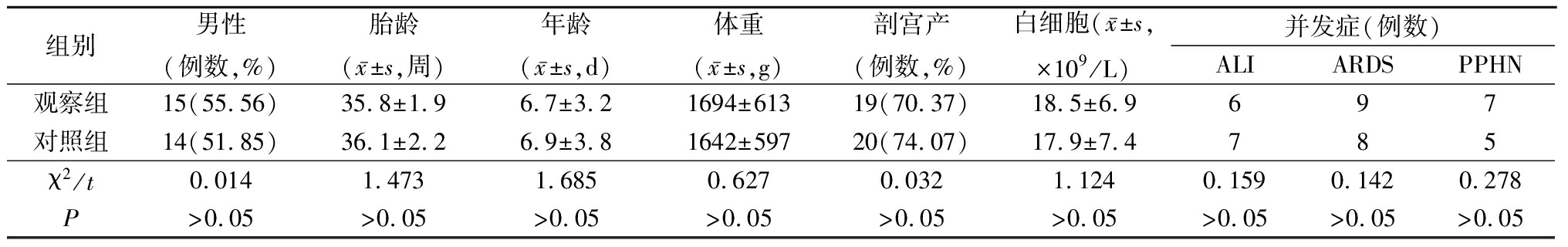
2.12组治疗前后呼吸功能指标比较 2组MAP、FiO2、OI及a/A在时点间、组间·时点间交互作用差异均具有统计学意义(P<0.05),在组间差异无统计学意义(P>0.05),见表2。
表2 2组治疗前后呼吸功能指标比较
Table2Comparison of respiratory function index between two groups before and after treatment![]()
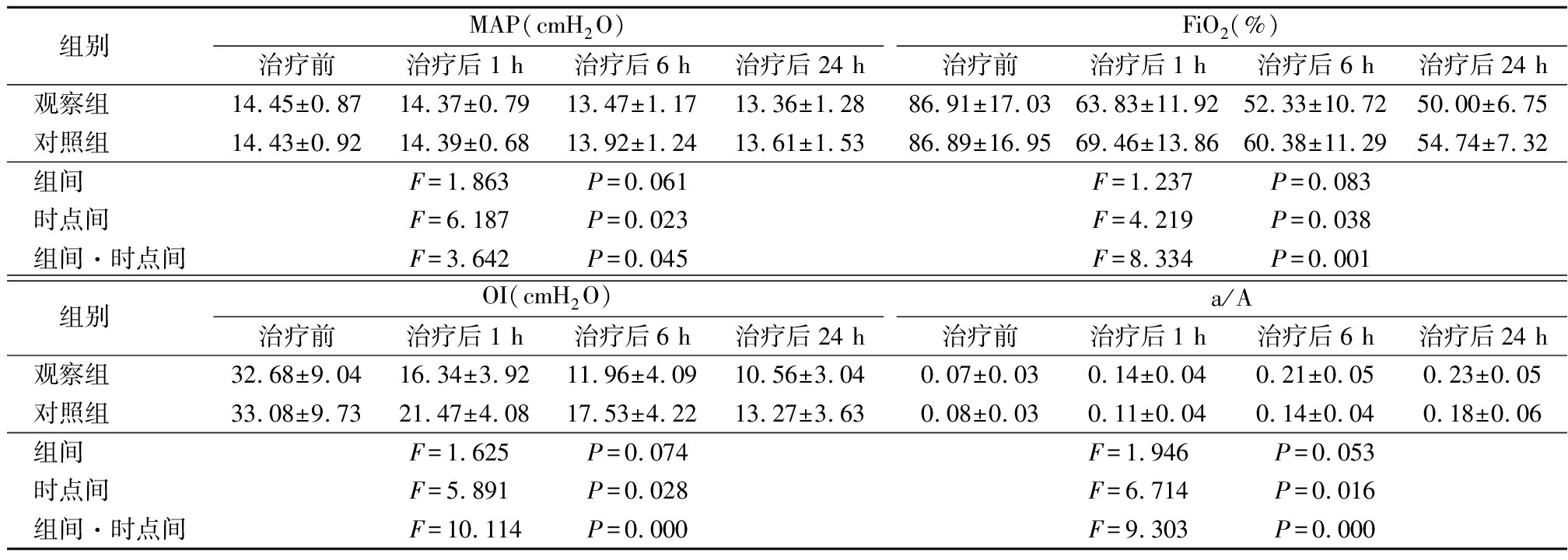
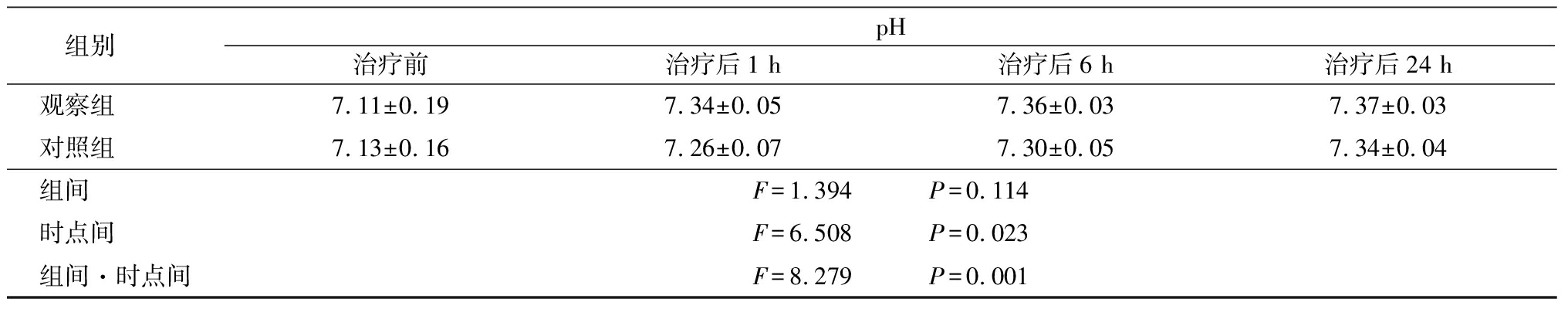
2.22组治疗前后血气指标比较 2组PaO2、PaCO2及pH值在时点间、组间·时点间交互作用差异均有统计学意义(P<0.05),在组间差异无统计学意义(P>0.05),见表3。
表3 2组治疗前后血气指标比较
Table3Comparison of blood gas indicators between two groups before and after treatment![]()
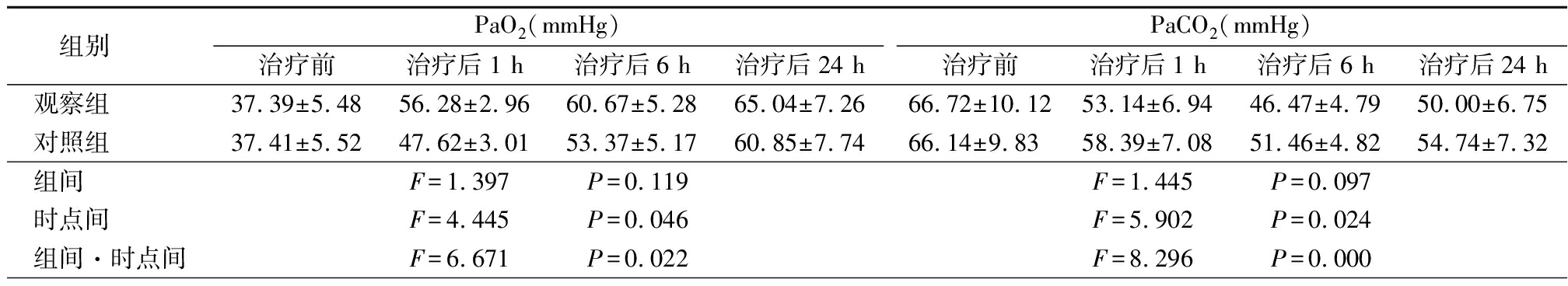
表3(续)
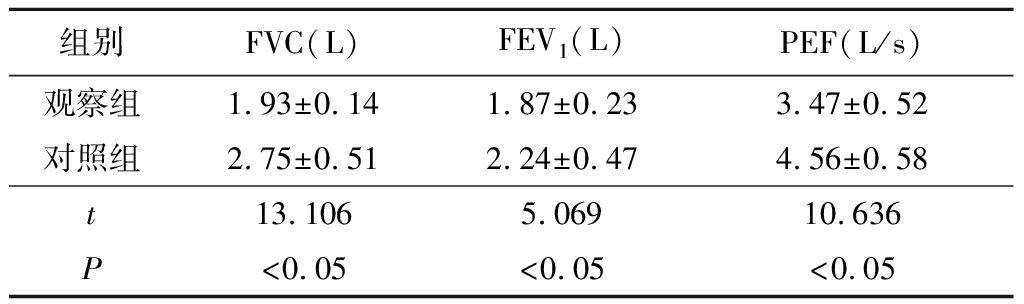
2.32组治疗后肺功能指标比较 观察组治疗后FVC、FEV1、PEF明显低于对照组,差异均有统计学意义(P<0.05),见表4。
表4 2组治疗后肺功能指标比较
Table4Comparison of lung function indicators between two groups after treatment![]()
2.42组治疗后重度肺炎相关临床体征消失时间比较 观察组治疗后重度肺炎相关的三凹征、肺部啰音、发热、发绀及鼻翼扇动等临床体征消失时间明显短于对照组,差异均有统计学意义(P<0.05),见表5。
表5 2组治疗后重度肺炎临床表现消失时间比较
Table5Comparison of disappeared time between two groups with severe pneumonia after treatment![]()
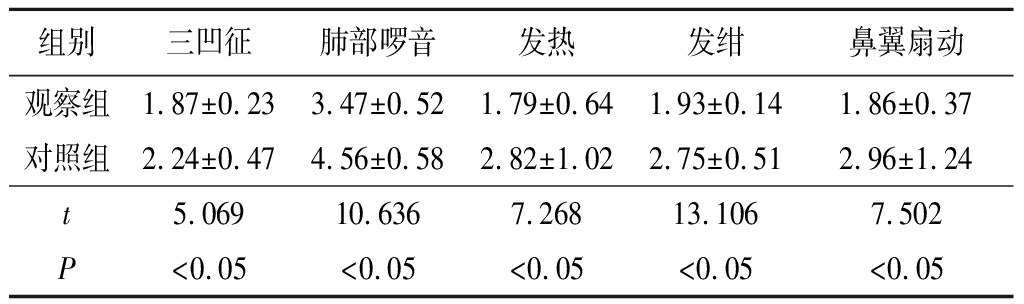
随着医疗水平的不断提高和临床研究的逐渐深入,现已证实吸入NO在治疗幼儿危重呼吸类疾病方面具有重要的临床意义,尤其是近年来,吸入NO在新生儿中的应用逐渐增多[9-10]。最近的一项研究表明,吸入NO可以抑制NF-κB介导的促炎性介质的释放,减少肺内中性粒细胞的聚集,进而减轻肺部炎症,同时还可以促进肺泡增殖,抑制肺纤维化[11]。此外,国内外的一些研究也证实,外源性NO对绿脓杆菌性肺炎、肺炎球菌性肺炎等均具有一定的抗菌作用[12-13]。然而,以往的研究多集中在吸入NO联合CMV治疗新生儿重症肺炎的相关并发症[14],关于吸入NO联合HFOV治疗新生儿重症肺炎的研究却较少,故本研究比较了吸入NO联合HFOV与单独应用HFOV治疗新生儿重症肺炎的临床效果,结果显示采用吸入NO联合HFOV治疗的观察组治疗后FVC、FEV1、PEF明显低于对照组,且观察组治疗后重度肺炎相关的三凹征、肺部啰音、发热、发绀及鼻翼扇动等临床体征消失时间明显短于对照组。提示吸入NO联合HFOV治疗不仅可以明显改善患儿的肺功能,还可以明显改善新生儿重症肺炎的临床症状。
重症肺炎是严重威胁婴幼儿,尤其是新生儿生命安全的一种常见儿科疾病,极易引起严重的多脏器功能障碍,包括ALI、ARDS和PPHN等[15]。这主要是由于新生患儿呼吸道较狭窄,肺泡数量较少且黏膜敏感,加之患儿的排痰和咳嗽能力相对较差,易使呼吸道被分泌的黏液阻塞[16-17]。值得注意的是,NO是一种选择性肺血管舒张剂,外源性NO经肺泡壁进入血管平滑肌细胞后能扩张血管,进而降低肺动脉压力,改善通气/血流比值和氧合指数[18]。已有研究表明吸入NO治疗新生儿持续肺动脉高压、新生儿低氧性呼吸衰竭等方面安全有效[19]。同时,最近的研究表明,HFOV采用的压力和潮气量均较小,可有效地降低CMV治疗所引起的气压伤和容积伤,不会增加发生气漏的风险[20]。本研究结果显示,2组治疗后MAP、FiO2、OI均明显低于治疗前,a/A明显高于治疗前,其时点间、组间·时点间交互作用差异均有统计学意义(P<0.05);2组治疗后PaO2和pH值明显高于治疗前,PaCO2明显低于治疗前,其时点间、组间·时点间交互作用差异也均有统计学意义(P<0.05)。提示吸入NO联合HFOV治疗可以明显改善呼吸指标和血气指标,这主要是由于NO对体循环血压不产生影响,而联合HFOV治疗能够使肺泡加速递送NO,进而可以更好地发挥吸入NO的抗菌作用。本研究观察组未出现明显的不良反应,且国外关于新生儿吸入NO的临床研究显示,采用吸入NO治疗的婴儿在18~24个月时进行运动及感觉等神经发育的评估,未发现有不良影响。这也提示吸入NO联合HFOV治疗新生儿重症肺炎是安全有效的。
综上所述,虽然新生儿重症肺炎的治疗难度依然较大,且病死率高,但随着对疾病的认识和治疗手段的增加,采取吸入NO联合HFOV可以明显改善患儿的呼吸功能和血气指标,并显著改善肺功能和重度肺炎相关的临床体征,具有一定临床应用和研究价值。
[参考文献]
[1] D′Aronco S,Simonato M,Vedovelli L,et al. Surfactant protein B and A concentrations are increased in neonatal pneumonia[J]. Pediatr Res,2015,78(4):401-406.
[2] 李新江,方艳伟,魏浩飞,等.早期持续性高容量血液滤过对重症急性胰腺炎急性肺损伤患者的影响[J].河北医科大学学报,2016,37(2):198-201.
[3] Peden WM,Richard JL,Trampel DW,et al. Mycotic Pneumonia and Meningoencephalitis due to Aspergillus terreus in a Neonatal Snow Leopard (Panthera uncia)[J]. J Wildlife Dis,2015,21(3):301-305.
[4] Roux DML,Myer L,Nicol MP,et al. Incidence and severity of childhood pneumonia in the first year of life in a South African birth cohort: the Drakenstein Child Health Study[J]. Lancet Glob Health,2015,3(2):e95.
[5] Ruan SY,Wu HY,Lin HH,et al. Inhaled nitric oxide and the risk of renal dysfunction in patients with acute respiratory distress syndrome: a propensity-matched cohort study[J]. Crit Care,2016,20(1):389.
[6] Sokol GM,Konduri GG,Van Meurs KP. Inhaled nitric oxide therapy for pulmonary disorders of the term and preterm infant[J]. Semin Perinatol,2016,40(6):356.
[7] Maitra S,Bhattacharjee S,Khanna P,et al. High-frequency ventilation does not provide mortality benefit in comparison with conventional lung-protective ventilation in acute respiratory distress syndrome: a meta-analysis of the randomized controlled trials[J]. Anesthesiology,2015,122(4):841-851.
[8] 邵民坤,周燕,杜坤,等.炎性指标联合检测在鉴别诊断新生儿感染中的临床评价[J].中华医院感染学杂志,2016,26(7):1639-1641.
[9] 龙小平,秦志强.无创与有创通气治疗慢性阻塞性肺疾病并严重呼吸衰竭的临床对照研究[J].河北医科大学学报,2011,32(9):1052-1055.
[10] Hawkes MT,Conroy AL,Opoka RO,et al. Inhaled nitric oxide as adjunctive therapy for severe malaria: a randomized controlled trial[J]. Malar J,2015,14(1):421.
[11] Finer NN,Evans N. Inhaled nitric oxide for the preterm infant: evidence versus practice[J]. Pediatrics,2015,135(4):754-756.
[12] 李培燕.78例新生儿吸入性肺炎的临床诊疗分析[J].河北医科大学学报,2015,36(2):159-161.
[13] Ruan SY,Huang TM,Wu HY,et al. Inhaled nitric oxide therapy and risk of renal dysfunction: a systematic review and meta-analysis of randomized trials[J]. Crit Care,2015,19(1):137.
[14] Asadi AK,S RC,Kim NH,et al. Inhaled nitric oxide alters the distribution of blood flow in the healthy human lung,suggesting active hypoxic pulmonary vasoconstriction in normoxia[J]. J Appl Physiol,2015,118(3):331-343.
RC,Kim NH,et al. Inhaled nitric oxide alters the distribution of blood flow in the healthy human lung,suggesting active hypoxic pulmonary vasoconstriction in normoxia[J]. J Appl Physiol,2015,118(3):331-343.
[15] Bhatraju P,Crawford J,Hall M,et al. Inhaled nitric oxide: Current clinical concepts[J]. Nitric Oxide,2015,50:114-128.
[16] Ye Q,Shao W,Shang S,et al. Epidemiological characteristics and immune status of children with Respiratory Syncytial Virus[J]. J Med Virol,2015,87(2):323.
[17] Ben-Shimol S,Greenberg D,Hazan G,et al. Differential impact of pneumococcal conjugate vaccines on bacteremic pneumonia versus other invasive pneumococcal disease[J]. Pediatr Infect Dis J,2015,34(4):409-416.
[18] Nahar K,Rashid J,Absar S,et al. Liposomal Aerosols of Nitric Oxide (NO) Donor as a Long-Acting Substitute for the Ultra-Short-Acting Inhaled NO in the Treatment of PAH[J]. Pharm Res,2016,33(7):1696-1710.
[19] Bronicki RA,Fortenberry J,Schreiber M,et al. Multicenter Randomized Controlled Trial of Inhaled Nitric Oxide for Pediatric Acute Respiratory Distress Syndrome[J]. J Pediatrics,2015,166(2):365-369.
[20] De LD,Costa R,Visconti F,et al. Oscillation transmission and volume delivery during face mask-delivered HFOV in infants: Bench and in vivo study[J]. Pediatr Pulm,2016,51(7):705-712.
YANG Li, CHEN Yan-hua, XU Feng-ling*
(Department of Pediatrics,Taizhou Peopie′s Hospital,Jiangsu Province,Taizhou225300,China)
[Abstract]ObjectiveTo investigate the clinical efficacy of inhaled nitric oxide(NO) combined with high frequency shock ventilation (HFOV) in the treatment of neonatal severe pneumonia.MethodsFrom January 2012 to December 2016, 54 children with severe neonatal severe pneumonia were enrolled in this study. They were randomly divided into observation group(inhaled NO combined with HFOV treatment) and control group(HFOV treatment), each group of 27 cases. The respiratory function index and blood gas index, and the lung function index after treatment and the time of disappearance of severe pneumonia-related clinical signs were recorded before and 1 h, 6 h and 24 h after treatment.ResultsThe mean airway pressure(MAP), inspired oxygen volume fraction(FiO2), oxygenation index(OI), and a/A interaction between time points and between groups and time points in the two groups were statistically significant(P<0.05). There was no significant difference between the groups(P>0.05). The differences in arterial oxygen partial pressure(PaO2), carbon dioxide partial pressure(PaCO2), and pH between the two groups were statistically significant(P<0.05). There was no significant difference between the groups(P>0.05). The forced vital capacity(FVC), forced expiratory volume in one second(FEV1), and peak expiratory flow(PEF)after treatment in the observation group were significantly lower than those in the control group(P<0.05). The time of disappearance of clinical signs such as three-indented sign, pulmonary rales, fever, cyanosis, and alar fan was significantly shorter in the observation group than in the control group. The difference was statistically significant(P<0.05).ConclusionInhaled nitric oxide combined with high frequency shock ventilation in the treatment of neonatal severe pneumonia can significantly improve the children′s respiratory function and blood gas index, and significantly improve the lung function and severe pneumonia-related clinical signs, has a certain clinical application and research value.
[Key words]pneumonia; nitric oxide; chest wall oscillation; infant, newborn
[收稿日期]2017-10-13;
[中图分类号]R563. 1
[文献标志码]A
[文章编号]1007-3205(2018)09-1038-05
[修回日期]2017-11-23
[基金项目]江苏大学医学临床科技发展基金(JLY20160152)
[作者简介]杨丽(1976-),女,江苏泰州人,江苏省泰州市人民医院副主任医师,从事新生儿疾病诊治研究。
*通讯作者。E-mail:2606644751@qq.com
(本文编辑:刘斯静)