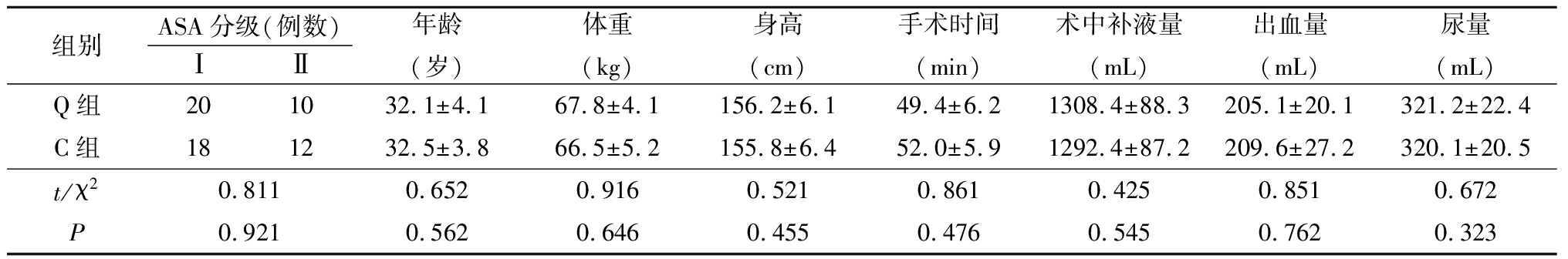
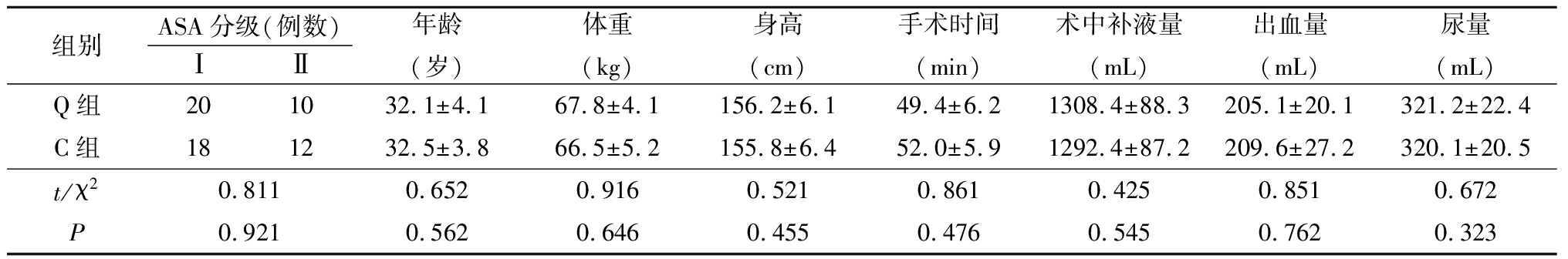
表1 2组一般情况比较
Table1Comparison of general data between two groups![]()
·论 著·
张隆盛,林旭林,张欢楷,杨 铎,林耿彬,黄志良
(广东省揭阳市人民医院麻醉科,广东 揭阳 522000)
[摘要] 目的探讨超声引导腰方肌阻滞(quadratus lumborum block,QLB)对剖宫产术术后镇痛效果的影响。方法选择择期行足月剖宫产术产妇60 例,随机分为QLB组(Q组)和对照组(C组)各30例。2组均采用腰硬联合麻醉,术后均行经静脉患者自控镇痛(patient controlled intravenous analgesia,PCIA)。Q组于术毕行超声引导双侧QLB,每侧注射0.25%罗哌卡因30 mL,C组不阻滞。记录手术时间、术中补液量、出血量及尿量。记录2组术后2,4,8,12,24,36,48 h静息和运动时VAS评分;记录术后首次按压镇痛泵时间、48 h内镇痛泵有效按压次数/实际按压次数比(D1/D2)和舒芬太尼用量;记录术后恢复情况;术后48 h随访并记录产妇对镇痛效果的满意度和镇痛期间不良反应发生情况。结果2组各时点静息和运动VAS评分均呈逐渐上升再下降趋势,且Q组低于C组,组间、时点间、组间·时点间交互作用差异均有统计学意义(P<0.05)。Q组术后首次按压镇痛泵时间明显延长,D1/D2明显升高,术后48 h内舒芬太尼用量明显减少(P<0.05)。Q组术后首次排气时间、进食普通食物时间、下床活动时间明显缩短(P<0.05)。Q组产妇对镇痛的满意度明显升高(P<0.05)。结论剖宫产术后实施超声引导QLB镇痛效果确切,能显著缓解产妇术后疼痛,减少阿片类药物使用,促进产妇快速康复同时提高满意度。
[关键词]麻醉和镇痛;剖宫产术;病人满意度 doi:10.3969/j.issn.1007-3205.2018.09.014
剖宫产术后切口疼痛给产妇带来多种不良影响,如影响产妇早期活动及快速康复、抑制乳汁分泌等。术后良好镇痛能有效缓解疼痛反应,产妇可早期下床,降低深静脉血栓发生率,有利于产妇的快速康复和泌乳[1-2]。目前临床上多采用硬膜外镇痛或静脉镇痛,硬膜外镇痛虽然效果确切但低血压、运动阻滞、尿储留、抑制胃肠道蠕动发生率高,而静脉镇痛效果差,且容易发生呼吸抑制、过度镇静、恶心呕吐等不良反应[3-4]。腹横肌平面阻滞目前已被证实在腹部术后镇痛领域有良好应用前景[5],Blanco等[6-7]在近年来发现一种新的区域阻滞技术——腰方肌阻滞(quadratus lumborum block,QLB),它被描述为后路腹横肌平面阻滞。QLB被广泛应用于腹部手术、髋部手术的复合麻醉及术后镇痛,但目前QLB用于剖宫产术后镇痛在国内至今鲜见报道。本研究探讨QLB对剖宫产术后镇痛的影响,旨在为产妇提供多模式镇痛方案。
1.1一般资料 选择2016年9月—2018年2月在我院择期行足月剖宫产术产妇60 例,年龄24~40岁,ASA 分级为Ⅰ或Ⅱ级,所有患者均无严重中枢或外周神经系统疾病、心血管系统疾病、肝肾疾病,无凝血功能异常、穿刺部位感染、脊柱畸形,无罗哌卡因或阿片类药物过敏史。按随机数字表法分为腰方肌阻滞组(Q组)和对照组(C组)各30例。2组产妇ASA分级、年龄、体重、身高、手术时间、术中补液量、出血量、尿量差异均无统计学意义(P>0.05),具有可比性,见表1。
本研究获得揭阳市人民医院伦理委员会批准(批件号:2017008);所有入组产妇均知情并签署知情同意书。
表1 2组一般情况比较
Table1Comparison of general data between two groups![]()
1.2麻醉方法 所有产妇术前常规禁饮禁食,入室后常规监测血压、心电图、脉搏血氧饱和度和心率,开放左上肢静脉通路,输注复方乳酸钠500 mL,鼻导管吸氧2~3 L/min。所有产妇均采用腰硬联合麻醉,所有穿刺操作均由同一位技术熟练的医师实施,产妇取侧卧位,选择L3~4间隙垂直正中穿刺。穿刺成功后明确脑脊液回流顺畅后注入腰麻药物,即1.0%罗哌卡因1.5 mL+脑脊液0.5 mL,腰麻针开口朝向头侧,匀速注药速度0.1 mL/s,注药后向头侧置入硬膜外导管,留置长度3 cm,妥善固定导管后让产妇平卧,根据麻醉效果硬膜外腔追加1.0%罗哌卡因6~8 mL,术中麻醉平面控制在T6~S5。术中根据血压、心率变化调整输液速度。若血压下降幅度超过基础值30%,静脉注射间羟胺0.25~0.50 mg或麻黄碱5~10 mg;心率低于50次/min,静脉注射阿托品0.5 mg。术毕2组产妇均行患者自控镇痛,配方如下:舒芬太尼2 μg/kg,昂丹司琼8 mg,加生理盐水稀释至100 mL,持续背景输注速率2 mL/h,单次剂量2 mL,锁定时间15 min。Q组于麻醉后监测治疗室内行超声引导下双侧QLB,每侧注射0.25%罗哌卡因30 mL,C组不实施QLB。
Q组产妇采用Blanco等[8]介绍的QLB 2法阻滞。产妇取侧卧位,消毒铺巾后用SonoSite M-turbo便携式超声仪及C60x低频凸阵探头(2~5 MHz),探头横向置于肋缘与髂棘之间,调整探头位置至清晰显示腰椎横突,可见围绕横突的三块肌肉:腰大肌在前,竖脊肌在后,腰方肌位于横突顶点,可在竖脊肌外侧或腰方肌后外侧找到背阔肌,注药位点位于腰方肌、背阔肌和竖脊肌组成的腰方肌后腰筋膜内三角。固定探头,用80 mm的22 G穿刺针在探头背侧进针,针尖由后外向前内,保持针与超声探头同一平面,清晰显示针尖针干,待针尖至注药位点后注射生理盐水5 mL,通过水分离再次确认针尖位置准确后,回抽无血无气体并将30 mL 0.25%罗哌卡因注入,注药后采用相同方法行对侧QLB,所有操作均由同一位麻醉医师完成,术后由另一位不知分组情况的麻醉医师观察并记录。
1.3观察指标 记录术后2,4,8,12,24,36,48 h静息及运动时视觉模拟评分法(Visual Analogue Scale,VAS)疼痛评分(0分,无痛;1~2分,偶有轻微痛;3~4分,常有轻微痛;5~9分,明显疼痛;10分,剧痛);记录术后首次按压镇痛泵时间、48 h内镇痛泵有效按压次数/实际按压次数比(D1/D2)和舒芬太尼用量;记录术后恢复情况(术后首次排气时间、进食普通食物时间、下床活动时间);术后48 h随访并记录产妇对镇痛效果的满意度(以表示满意的产妇例数百分比评价。满意,无痛或轻度疼痛,日常活动不受限,情绪稳定;一般,中度疼痛但能忍受,日常活动轻度受限,情绪稳定;不满意,中重度疼痛不能忍受,活动明显受限,情绪低落甚至烦躁)和镇痛期间不良反应发生情况(包括恶心呕吐、低血压等)。
1.4统计学方法 应用SPSS 20.0统计软件处理数据。计量资料比较分别采用两独立样本的t检验和重复测量的方差分析;计数资料比较采用χ2检验。P<0.05 为差异有统计学意义。
2.12组产妇术后不同时点静息和运动VAS评分比较 2组各时点静息和运动VAS评分均呈逐渐上升再下降趋势,且Q组低于C组,组间、时点间、组间·时点间交互作用差异均有统计学意义(P<0.05),见表2。
表2 2组术后不同时点静息和运动VAS评分比较
Table2Comparison of VAS and Ramsay scores at different times between two groups ![]() 分)
分)
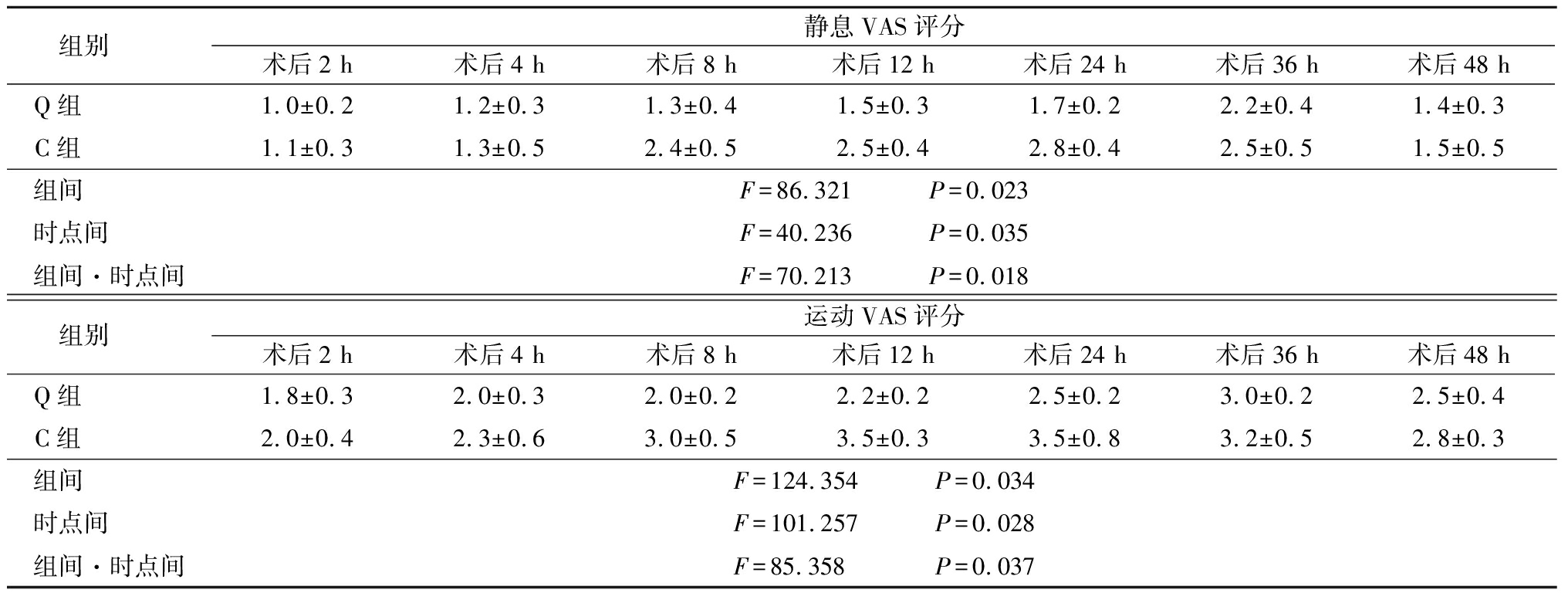
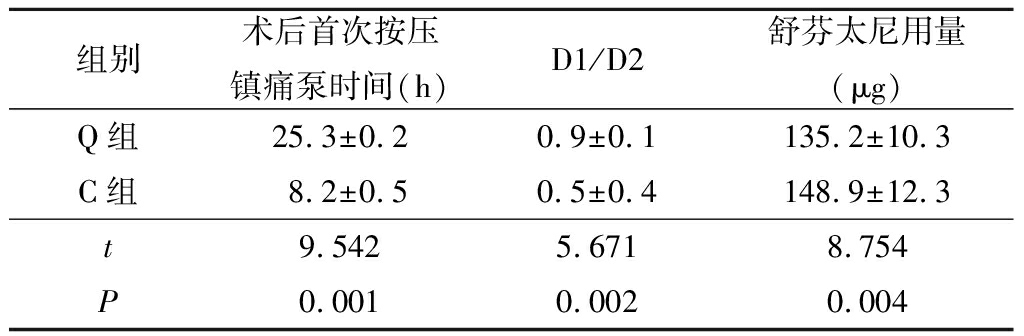
2.22组产妇术后镇痛药物使用情况比较 与C组比较,Q组术后首次按压镇痛泵时间明显延长,D1/D2明显升高,术后48 h内舒芬太尼用量明显减少(P<0.05),见表3。
表3 2组术后镇痛药物使用情况比较
Table3Comparison of the use of postoperative analgesic drugs between two groups![]()
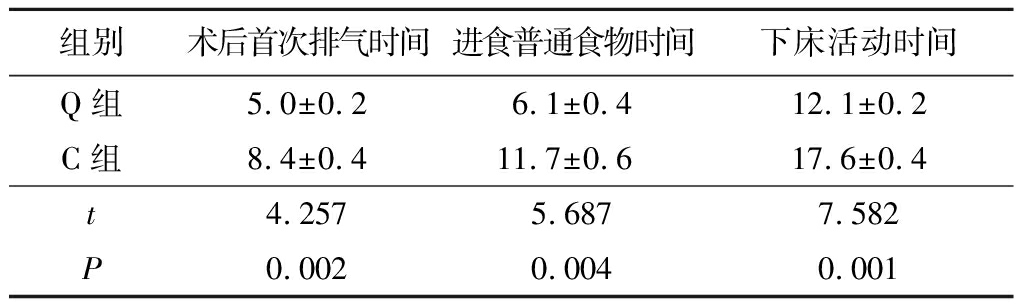
2.32组产妇术后恢复情况相关指标比较 与C组比较,Q组术后首次排气时间、进食普通食物时间、下床活动时间明显缩短(P<0.05),见表4。
表4 2组术后恢复情况相关指标比较
Table4Comparison of postoperative recovery between two groups![]()
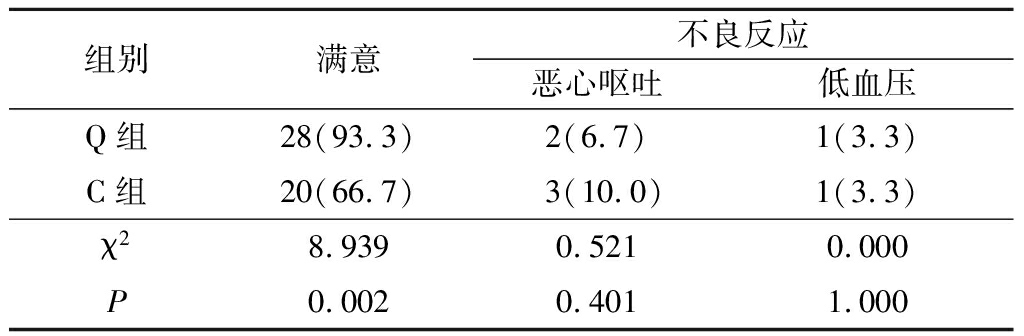
2.42组产妇术后镇痛满意度及不良反应比较 与C组比较,Q组产妇对镇痛效果的满意度明显升高(P<0.05),2组产妇不良反应发生情况(恶心呕吐、低血压)差异均无统计学意义(P>0.05),见表5。
表5 2组术后镇痛满意度及不良反应比较
Table5Comparison of postoperative analgesia satisfaction and adverse reaction between two groups(n=30,例数,%)
剖宫产术后完善的镇痛能有效缓解疼痛反应,促进产妇快速康复。目前临床上常规采用静脉镇痛或硬膜外镇痛。阿片类药物静脉镇痛容易发生呼吸抑制、瘙痒、过度镇静、恶心呕吐等不良反应[3]。硬膜外镇痛虽然效果优于静脉镇痛,但低血压、运动阻滞、尿储留、抑制胃肠道蠕动等不良反应发生率高。快速康复外科术后镇痛提倡多模式镇痛方案[9],神经阻滞技术是术后多模式镇痛的一种安全有效的补充方法。
本研究Q组术后8,12,24 h VAS评分明显低于C组,且首次按压镇痛泵时间为(25.3±0.2) h,表明QLB单次注药维持时间约24 h。这与以往研究结果一致。Sebbag等[10]发现,剖宫产术后行单次QLB,产妇术后24 h内不需要额外吗啡镇痛。Kadam[11]发现,单次QLB可降低患者24 h的VAS评分和阿片类药物使用需求。Blanco等[8]发现,剖宫产术后行单次QLB,术后镇痛持续时间长达48 h,这可能与局麻药种类或容量有关。罗哌卡因是长效酰胺类局麻药,神经毒性和心血管毒性低。本研究选用0.25%罗哌卡因;有文献报道,用于外周神经阻滞的罗哌卡因适宜浓度为0.2%~0.5%[12];还有文献报道,单次QLB常用0.25%罗哌卡因20~30 mL,镇痛持续时间为18~24 h,或持续48 h以上[6,8]。本研究2组术后2,4 h VAS评分差异无统计学意义,可能与椎管内罗哌卡因作用未完全消退有关。
前腹壁皮肤、肌肉及壁层腹膜是由低位的胸腰段神经(T6~L1)支配,这些神经前支穿出椎间孔后,在肋弓处越过肋缘并穿入侧腹壁,行走于腹横肌与腹内斜肌之间。Blanco等[8]指出腰方肌与背阔肌、竖脊肌、腰大肌、腹壁肌之间有一个潜在的解剖腔隙,QLB则根据注药位点的不同分为QLB 1、QLB 2、QLB 3三种入路。QLB 1注药位点位于腰方肌前外侧,腹横筋膜浅层,称为外路QLB。QLB 2注药位点位于腰方肌后侧和背阔肌之间,称为后路QLB。QLB 3注药位点位点腰方肌前内侧与腰大肌之间,称为前路QLB。Carline等[13]通过在尸体上注射染料观察扩散情况,发现QLB 1、QLB 2和QLB 3均能扩散至腹横肌平面阻滞包含的神经,QLB 1、QLB 2有时还扩散至椎旁区域,沿胸腰筋膜向上扩散,QLB 3则更易扩散至L1~3椎旁,甚至扩散至腰丛区域。Spence等[14]发现QLB 2入路测得阻滞平面为T7~L1,本研究采用此入路,但由于产妇采用的是椎管内麻醉且术后联合患者自控镇痛多模式镇痛,故无法对术后各时点进行QLB平面测试。
快速康复最关键的3个技术指标是良好的术后镇痛、早期下床活动、早期恢复胃肠功能。本研究Q组产妇术后首次排气时间、下床活动时间和进食普通食物时间明显短于C组,48 h内舒芬太尼用量明显少于C组,48 h产妇镇痛满意度明显高于C组。提示剖宫产术后采用QLB,能缩短产妇下床活动时间,减少阿片类药物使用,促进胃肠功能早期恢复,产妇满意度较高,更符合快速康复的目标。
QLB被广泛用于腹部术后的镇痛。Shaaban等[15]报道结直肠切除术后行QLB,明显减少阿片类药物用量。Cardoso等[16]报道胃切除术后行QLB 2,可明显缓解术后疼痛同时避免阿片类药物的应用。还有报道QLB还可用于缓解疝修补术后疼痛[17]。此外,研究还表明,QLB能用于全髋关节置换术后镇痛,提供较长时间的良好镇痛且不引起患者肌力减弱[18]。作为新兴的躯干阻滞技术,QLB比腹横肌平面阻滞更有优势。在Blanco等[7]的随机对照研究中,76例剖宫产产妇分别采用QLB或腹横肌平面阻滞行术后镇痛,发现术后48 h QLB组较腹横肌平面组更能减少术后阿片类药物的应用。Murouchi等[19]发现,全身麻醉腹腔镜卵巢手术患者术后分别行腹横肌平面阻滞或QLB,QLB镇痛时间较腹横肌平面阻滞长。
综上所述,剖宫产术后实施超声引导QLB镇痛效果确切,能显著缓解产妇术后疼痛,减少阿片类药物的使用,促进产妇快速康复同时提高满意度,其可作为多模式镇痛重要组成部分,值得在临床上推广。
[参考文献]
[1] Fuchs F,Benhamou D. Post-partum management after cesarean delivery Guidelines for clinical practice[J]. J Gynecol Obstet Biol Reprod(Pairs),2015,44(10):1111-1117.
[2] Abdallah FW,Laffey JG,Halpern SH,et al. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions:a meta-analysis[J]. Br J Anaesth,2013,111(5):721-735.
[3] Andziak M,Beta J,Barwijuk M,et al. Efficacy and tolerability of intravenous morphine patient-controlled analgesia(PCA) in women undergoing cesarean delivery[J]. Ginekol Pol,2015,86(6):453-456.
[4] 张荣.罗哌卡因复合舒芬太尼在分娩镇痛中的应用[J].河北医科大学学报,2016,37(3):337-339.
[5] Fusco P,Scimia P,Paladini G,et al. Transversus abdominis plane block for analgesia after Cesarean delivery.A systematic review[J]. Minerva Anestesiol,2015,81(2):195-204.
[6] Blanco R,Ansari T,Girgis E. Quadratus lumborum block for postoperative pain after caesarean section:a randomised controlled trial[J]. Eur J Anaesthesiol,2015,32 (11):812-818.
[7] Blanco R,Ansari T,Riad W,et al. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery:a randomized controlled trial[J]. Reg Anesth Pain Med,2016,41(6):757-762.
[8] Blanco R,Ansari T,Girgis E. Quadratus lumborum block for postoperative pain after caesarean section:a randomised controlled trial[J]. Eur J Anaesthesiol,2015,32(11):812-818.
[9] 韩向真,康凯,耿倩,等.无痛管理模式在全膝关节置换术后的应用[J].河北医科大学学报,2017,38(3):290-292,296.
[10] Sebbag I,Qasem F,Dhir S. Ultrasound guided quadratus lumborum block for analgesia after cesarean delivery:case series[J]. Rev Bras Anestesiol,2017,67(4):418-421.
[11] Kadam VR. Ultrasound-guided quadratus lumborum block as a postoperative analgesic technique for laparotomy[J]. J Anaesthesiol Clin Pharmacol,2013,29(4):550-552.
[12] 王琳,徐铭军,魏江.超声引导腹横肌平面阻滞对剖宫产术后镇痛的影响[J].临床麻醉学杂志,2016,32(7):661-664.
[13] Carline L,McLeod GA,Lamb C. A cadaver study comparing spread of dye and nerve involvement after three different quadratus lumborum blocks[J]. Br J Anaesth,2016,117(3):387-394.
[14] Spence NZ,Olszynski P,Lehan A,et al. Quadratus lumborum catheters for breast reconstruction requiring transverse rectus abdominis myocutaneous flaps[J]. J Anesth,2016,30(3):506-509.
[15] Shaaban M,Esa WA,Maheshwari K,et al. Bilateral continuous quadratus lumborum block for acute postoperative abdominal pain as a rescue after opioid-induced respiratory depression[J]. A A Case Rep,2015,5(7):107-111.
[16] Cardoso JM,S M,Reis H,et al. Type Ⅱ Quadratus Lumborum block for a sub-total gastrectomy in a septic patient[J]. Rev Bras Anestesiol,2018,68(2):186-189.
M,Reis H,et al. Type Ⅱ Quadratus Lumborum block for a sub-total gastrectomy in a septic patient[J]. Rev Bras Anestesiol,2018,68(2):186-189.
[17] Carvalho R,Segura E,Loureiro MD,et al. Quadratus lumborum block in chronic pain after abdominal hernia repair:case report[J]. Braz J Anesthesiol,2017,67(1):107-109.
[18] Hockett MM,Hembrador S,Lee A. Continuous quadratus lumborum block for postoperative pain in total hip arthroplasty:A Case Rep[J]. A A Case Rep,2016,7(6):129-131.
[19] Murouchi T,Iwasaki S,Yamakage M. Quadratus lumborum block: analgesic effects and chronological ropivacaine concentrations after laparoscopic surgery[J]. Reg Anesth Pain Med,2016,41(2):146-150.
ZHANG Long-sheng, LIN Xu-lin, ZHANG Huan-kai,YANG Duo, LIN Geng-bin, HUANG Zhi-liang
(Department of Anesthesiology,Jieyang People′s Hospital,Guangdong Province,Jieyang522000,China)
[Abstract]ObjectiveTo investigate the effect of ultrasound-guided quadratus lumborum block(QLB) on the efficacy postoperative analgesia in parturient woman undergoing caesarean delivery.MethodsThere were 60 parturient in this study who were underwent full term cesarean section. Parturient woman were randomly divided into two groups:QLB group(Q group,n=30) and control group(C group,n=30).Two groups were treated by combined spinal epidural anesthesia, and all parturient woman were treated with PCIA after operation.After cesarean delivery,bilateral of ultrasound-guided QLB were performed,30 ml of 0.25% ropivacaine was injected in each side in Q group, while QLB was not done in C group. The time of operation, the amount of fluid infusion, the amount of bleeding and the volume of urine were recorded. The scores of resting and exercise VAS were recorded at 2, 4, 8, 12, 24, 36 and 48 h after operation.The time of the first press analgesia pump, the number of successfully doses(D1) and the number of attempts(D2) within 48 h, the amount of sufentanil within 48 h were recorded. D1/D2 was calculated. Postoperative recovery was recorded. The satisfaction of the parturient woman on the analgesic effect and the adverse reaction during the analgesia period were recorded at 48 hr postoperatively.ResultsThe VAS scores of the two groups at each time point were gradually rising and then decreasing, and the Q group was lower than the C group. The differences between intergroup, time point and interaction of intergroup and time point of two groups had the statistically significant. The first exhaust time,the time to eat ordinary food and the time to get out of bed after the operation were significantly lower,while the time of the first press analgesia pump, the value of D1/D2, the degree of satisfaction with analgesia were significantly higher in the Q group than those in C group(P<0.05).ConclusionAfter cesarean section, the effect of ultrasound-guided QLB analgesia is accurate, which can significantly alleviate the postoperative pain, reduce the use of opioids, promote rapid recovery of maternal and improve satisfaction.
[Key words]anesthesia and analgesia; cesarean section; patient satisfaction
[收稿日期]2018-03-27;
[中图分类号]R614.4
[文献标志码]A
[文章编号]1007-3205(2018)09-1053-05
[修回日期]2018-04-23
[基金项目]揭阳市卫生医疗科技项目(2017YL020)
[作者简介]张隆盛(1986-),男, 广东揭阳人,广东省揭阳市人民医院主治医师,医学学士,从事临床麻醉学研究。
(本文编辑:许卓文)