骨骺骨髓炎是一种骨骺的感染性疾病,该疾病可造成骨骺早闭、骨坏死缺损、关节畸形等后果,婴儿在患病初期的临床表现不典型,常表现为低热、局部红肿、肢体假瘫等症状,容易误诊,可能会出现难以治愈的后遗畸形。目前手术方式多为关节切开冲洗引流+干骺端钻孔减张术、单纯关节冲洗引流。干骺端减张术是使用电钻及克氏针对干骺端行钻孔减张,之后在关节内置入引流管;封闭式冲洗引流术则不进行减张,只是清理坏死组织后,置入引流管。本研究回顾性分析骨骺骨髓炎的3种治疗方式,评估患儿的肢体功能恢复情况,旨在为临床诊治提供参考。
1 资料与方法
1.1 一般资料 选自2009—2016年我院确诊为骨骺骨髓炎的患儿90例,按治疗方式分为3组各30例,A组行关节切开冲洗引流+干骺端钻孔减张术,B组行单纯冲洗引流术,C组未行手术治疗。由于部分病例失随访以及数据测量不健全,最终每组剩21例,其中各含肩关节8例、髋关节7例、膝关节6例。血常规显示白细胞平均值为17.68×109/L,血沉平均值32.14 mm/1 h、C反应蛋白平均值68.35 mg/L,均高于正常值,且有病变部位红肿、关节疼痛、皮温升高、肢体活动受限等情况,体温波动于37.8~39.2 ℃之间。X线显示骨骺内密度不均匀、干骺端骨质密度减低,周围软组织肿胀。MRI显示关节间隙及周围软组织高信号,骨骺内可见片状低信号或高信号,干骺端可见高信号,并伴有周围脓肿形成。
1.2 方法 手术治疗前测量患儿关节的活动范围,手术方式为切开引流,将关节切开后,引流出脓液,并留取标本送细菌培养或病理检查,用生理盐水冲洗关节腔后,探查骨骺及干骺端的骨质情况,如骨骺颜色变暗或存在虫噬样改变,则在干骺端行钻孔减张,并将剪有侧孔的引流管置入关节腔内,固定引流管并缝合关节腔周围软组织。术后记录患儿拔管时间,并定期复查X线及血液生化指标,术后6个月复诊时再次测量患儿关节的活动范围。
1.3 统计学方法 应用PEMS 3.2医学统计软件分析数据。计量资料比较分别采用F检验、SNK-q检验、两独立样本的t检验和配对t检验。P<0.05为差异有统计学意义。
2 结 果
2.1 3组治疗前后肩关节活动度比较 治疗前,3组外展、前屈和后伸活动度差异均无统计学意义(P>0.05);治疗后6个月,A组和B组肩关节外展、前屈和后伸活动度,C组的外展和后伸活动度均较治疗前明显增加(P<0.05),A组和B组 外展、前屈和后伸活动度均较C组增加,A组又均较B组增加(P<0.05)。见表1,图1,2。
Table 1 Comparison of shoulder range of motion before and after treatment among three groups
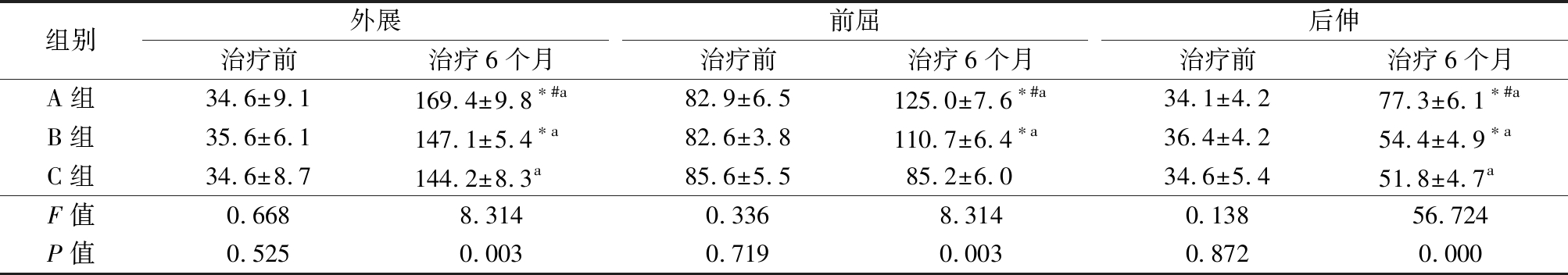
组别外展治疗前治疗6个月前屈治疗前治疗6个月后伸治疗前治疗6个月A组34.6±9.1169.4±9.8∗#a82.9±6.5125.0±7.6∗#a34.1±4.277.3±6.1∗#aB组35.6±6.1147.1±5.4∗a82.6±3.8110.7±6.4∗a36.4±4.254.4±4.9∗aC组34.6±8.7144.2±8.3a85.6±5.585.2±6.034.6±5.451.8±4.7aF值0.6688.3140.3368.3140.13856.724P值0.5250.0030.7190.0030.8720.000
*P值<0.05与C组比较 #P值<0.05与B组比较(SNK-q检验) aP值<0.05 与治疗前比较(配对t检验)
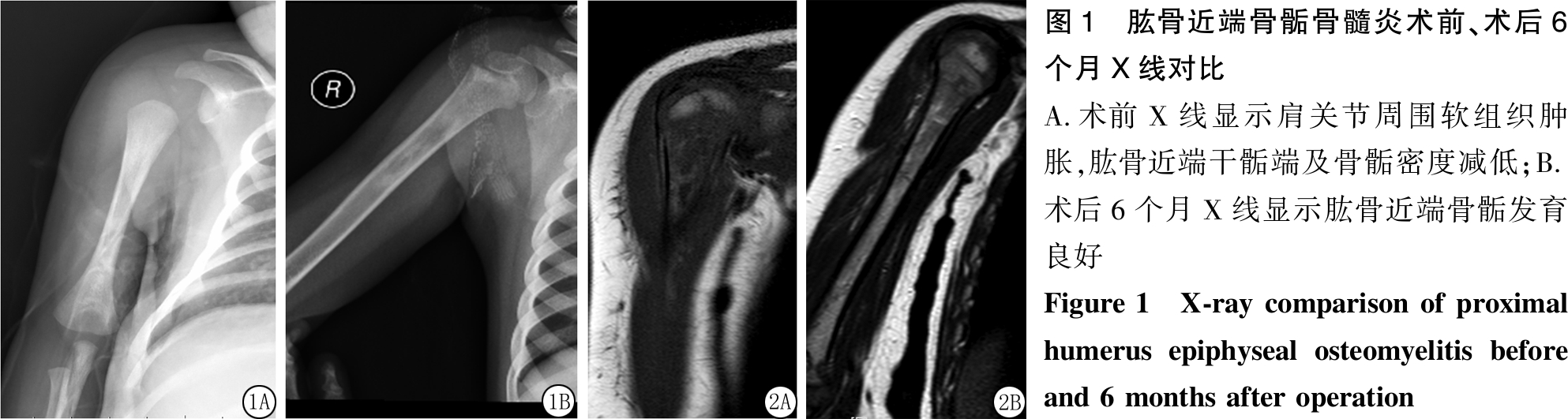
图1 肱骨近端骨骺骨髓炎术前、术后6个月X线对比 A.术前X线显示肩关节周围软组织肿胀,肱骨近端干骺端及骨骺密度减低;B.术后6个月X线显示肱骨近端骨骺发育良好Figure 1 X-ray comparison of proximal humerus epiphyseal osteomyelitis before and 6 months after operation
图2 肱骨近端骨骺骨髓炎术前、术后6个月MRI对比
A.术前MRI显示肱骨近端及骨骺密度不均匀;B.术后6个月MRI显示肱骨近端仍存在密度不均匀,但骨骺发育良好
Figure 2 MRI comparison of proximal humerus epiphyseal osteomyelitis before and 6 months after operation
2.2 3组治疗前后髋关节活动度比较 治疗前,3组髋关节屈曲、外展和内收活动度差异均无统计学意义(P>0.05);治疗后6个月,3组髋关节屈曲、外展和内收活动度均较治疗前明显增加,A组和B组屈曲、外展活动度均较C组增加(P<0.05),但3组内收活动度差异无统计学意义(P>0.05)。见表2,图3,4。
Table 2 Comparison of hip range of motion before and after treatment among three groups
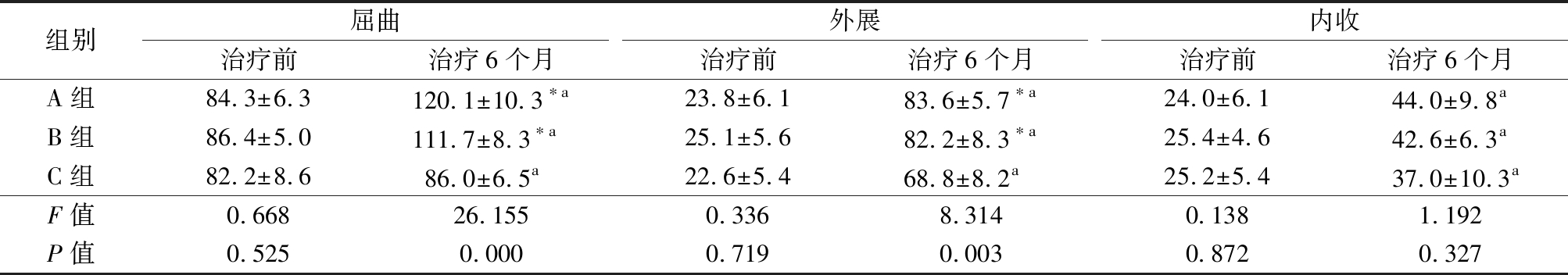
组别屈曲治疗前治疗6个月外展治疗前治疗6个月内收治疗前治疗6个月A组84.3±6.3120.1±10.3∗a23.8±6.183.6±5.7∗a24.0±6.144.0±9.8aB组86.4±5.0111.7±8.3∗a25.1±5.682.2±8.3∗a25.4±4.642.6±6.3aC组82.2±8.686.0±6.5a22.6±5.468.8±8.2a25.2±5.437.0±10.3aF值0.66826.1550.3368.3140.1381.192P值0.5250.0000.7190.0030.8720.327
*P值<0.05与C组比较 #P值<0.05与B组比较(SNK-q检验) aP值<0.05与治疗前比较(配对t检验)
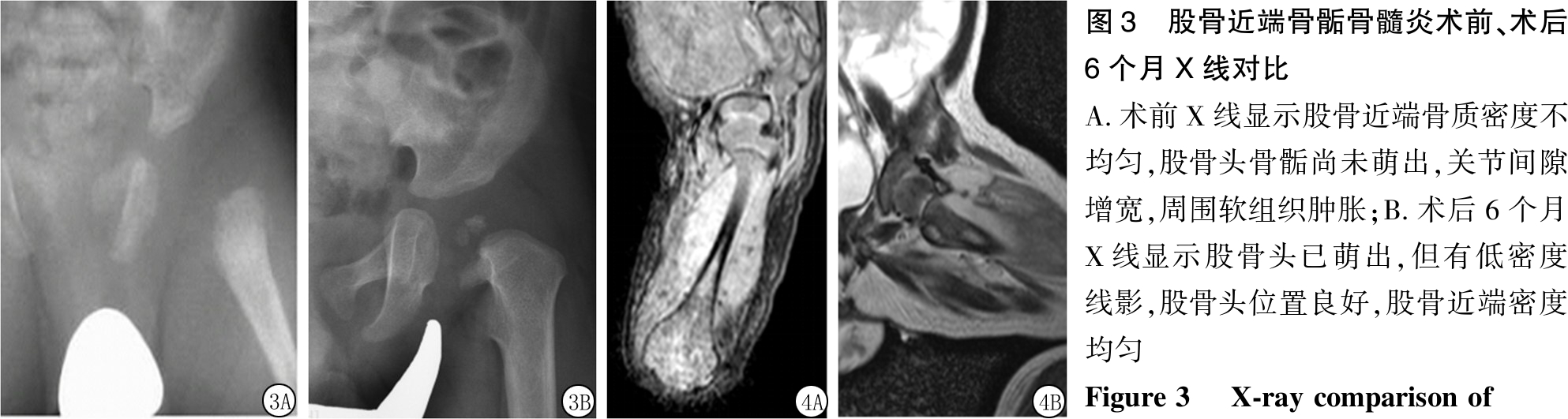
图3 股骨近端骨骺骨髓炎术前、术后6个月X线对比 A.术前X线显示股骨近端骨质密度不均匀,股骨头骨骺尚未萌出,关节间隙增宽,周围软组织肿胀;B.术后6个月X线显示股骨头已萌出,但有低密度线影,股骨头位置良好,股骨近端密度均匀 Figure 3 X-ray comparison of
proximal femoral epiphyseal osteomyelitis before and 6 months after operation
图4 股骨近端骨骺骨髓炎术前、术后6个月MRI对比
A.术前MRI显示股骨近端及骨骺密度不均匀,周围软组织高信号;B.术后6个月MRI显示股骨头及股骨近端密度较为均匀
Figure 4 MRI comparison of proximal femoral epiphyseal osteomyelitis before and 6 months after operation
2.3 3组治疗前后膝关节活动度、住院时间和拔管时间比较 治疗前,3组膝关节活动度差异无统计学意义(P>0.05);治疗后6个月,3组膝关节活动度均较治疗前明显增加(P<0.05),但3组间膝关节活动度差异无统计学意义(P>0.05)。A组和B组住院时间均少于C组,A组又少于B组,A组拔管时间少于B组(P<0.05)。见表3,图5,6。
Table 3 Comparison of knee joint of motion before and after treatment length of hospital stay and extubation among three groups
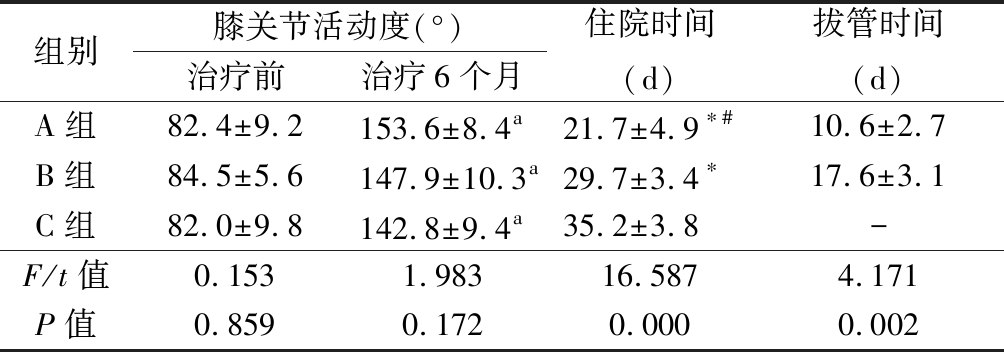
组别膝关节活动度(°)治疗前治疗6个月住院时间(d)拔管时间(d)A组82.4±9.2153.6±8.4a21.7±4.9∗#10.6±2.7B组84.5±5.6147.9±10.3a29.7±3.4∗17.6±3.1C组82.0±9.8142.8±9.4a35.2±3.8-F/t值0.1531.98316.5874.171P值0.8590.1720.0000.002
*P值<0.05与C组比较 #P值<0.05与B组比较(SNK-q检验) aP值<0.05与治疗前比较(配对t检验)
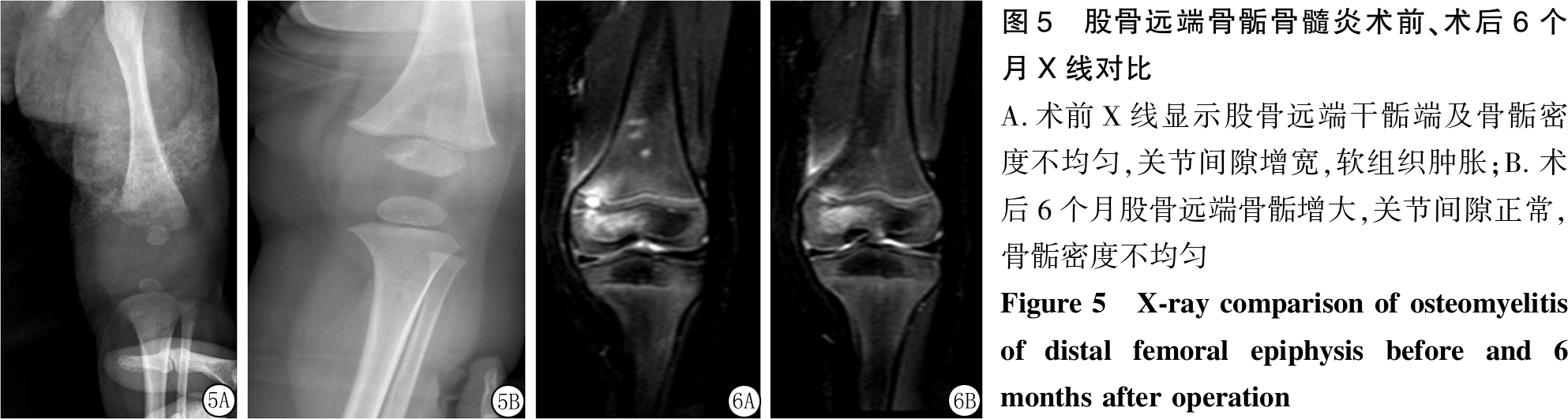
图5 股骨远端骨骺骨髓炎术前、术后6个月X线对比A.术前X线显示股骨远端干骺端及骨骺密度不均匀,关节间隙增宽,软组织肿胀;B.术后6个月股骨远端骨骺增大,关节间隙正常,骨骺密度不均匀 Figure 5 X-ray comparison of osteomyelitis of distal femoral epiphysis before and 6 months after operation
图6 股骨远端骨骺骨髓炎术前、术后6个月MRI对比
A.术前MRI显示股骨远端干骺端及骨骺密度不均匀,可见高信号影;B.术后6个月股骨远端干骺端高信号影消失,骨骺密度不均匀,但高信号影显著减弱
Figure 6 MRI comparison of osteomyelitis of distal femoral epiphysis before and 6 months after operation
3 讨 论
骨骺是儿童出生后在不同的时间内出现的二次骨化中心,骺板又称为生长板,其发生较长骨本身晚,稍迟于骨骺的发育。骺板可根据组织学及功能特点分为静止层、增殖层、肥大层。其中静止层与二次骨化中心相邻,此区域相对无明显活动性,故不参与骨质的纵向生长,但是可以产生基质以及具有储备的功能。增殖层是软骨细胞复制和生长区域,此区域代谢率较高,血氧和糖原供应丰富,三磷酸腺苷和骨胶原可使骨骼快速生长[1]。肥大层有肥大的软骨细胞,随着软骨细胞的增大,为钙化作准备。干骺端是血管、骨形成和再塑性的区域,该部位清除了钙化的基质,形成编织骨,并由板状骨代替。骨质的末端包括骺板和干骺端,是最容易发生感染、肿瘤、骨折等损伤的部位。骺板的血运来源于骺血管、干骺端血管、软骨周围血管。干骺端的血管主要来自于营养动脉[2],软骨周围的小血管也支配干骺端的边缘部分,这两个血运的终端形成血管襻,小的静脉襻末端形成静脉窦。在生后数个月内存在跨骺板的血管,此血管于干骺端血管形成吻合支,二次骨化中心形成和长大后则很少见到跨骺板的血管,是因为此时已有软骨下骨板形成[3]。
手术方法是切开引流、钻孔减张。病灶部位的骨骺、干骺端及周围软组织已经受到了炎症的破坏,手术中更不要大范围地剥离骨膜,以免影响骨皮质的血运。干骺端钻孔需要选择适当型号的克氏针,本研究中提到的钻孔减张,针对1岁以内的儿童使用的是2.0 mm或1.6 mm的克氏针,如较大型号的克氏针会消弱病骨的硬度[4],由于病灶部位炎症的存在,会出现骨质不愈合[5],甚至可以导致严重的病理性骨折,如果出现病理性骨折,骨质愈合过程将会很漫长[6]。有时可以通过术中C形臂透视进行局部的定位,以求更准确的钻孔部位。在手术操作过程中要避免损伤骺板,如果进一步损伤骺板,会对患儿日后功能恢复及肢体发育造成较大影响。手术钻孔减张可以有效地减轻干骺端的压力,有利于感染控制,同时降低骨髓腔内的压力,促进病变部位的血液循环,也可以减少血栓形成的机会[7],这样对病变部位的抗生素有效浓度是有利的。在清理病灶部位坏死组织及脓液后,用生理盐水反复冲洗,留取坏死组织和脓液送细菌培养+药敏,之后将引流管置入关节内,用于持续冲洗引流[8]。
行关节切开冲洗引流+干骺端钻孔减张术的患儿中,术后拔除引流管时间10~18 d,住院时间14~27 d,其中血培养或脓液培养均为阳性。行关节冲洗引流的患儿中,有部分患儿血培养或脓液培养为阴性,考虑与入院之前已行抗生素治疗有关[9-10],术后拔除引流管时间16~27 d,住院26~34 d。本研究结果显示,对于肩关节、髋关节及膝关节的功能恢复,行切开引流+干骺端钻孔减张术的患儿好于单纯行切开引流术的患儿。通过对比研究,切开引流+干骺端钻孔减张,可以有效地缩短冲洗引流的时间、拔除引流管,减少患儿的痛苦,有助于病情的恢复。缩短引流管拔除时间,一期缝合伤口,可缩短疗程及住院时间,对防治院内交叉感染、改善局部血运供应、预防骨组织坏死、降低致残率等均有帮助[11-12]。未行手术治疗的患儿,其中大部分血培养或脓液培养为阴性,这与入院之前已行相关治疗有关[13-14],该组患儿在入院时骨骺已经受到不可逆的破坏,且患儿体温及局部症状均无明显异常,此时手术已无意义[15-16]。其住院时间31~40 d。6个月之后随诊,肩关节、髋关节及膝关节功能虽均有所恢复,但较行手术治疗的患儿仍有较大的差距。
本研究还对 3组患儿的术后拔管时间、住院时间及关节活动范围进行了比较,行关节切开冲洗引流+骨骺及干骺端钻孔减张术的A组可以有效减轻干骺端张力,充分引流,刺激干骺端血运恢复,患儿住院时间及术后拔管时间明显缩短,术后长期随诊,肩关节、髋关节及膝关节功能恢复程度好于单纯行切开引流术的B组患儿和未行手术治疗的C组患儿。
本研究结果提示,对于已出现化脓性表现的骨骺骨髓炎患儿,除了及时明确诊断、足量足疗程使用抗生素之外,积极行外科手术治疗亦显得尤为重要。手术方式为关节切开引流+干骺端钻孔减张,该术式可以有效减轻骨骺及干骺端的压力,并使病灶部位得到较为充分的引流,从而促进疾病的恢复、缩短疗程,并降低该疾病的致残率。
[1] Hwang HJ,Jeong WK,Lee DH,et al.Acute primary hematogenous osteomyelitis in the epiphysis of the distal tibia:a case report with review of the literature[J]. J Foot Ankle Surg,2016,55(3):600-604.
[2] Ceroni D,Belaieff W,Cherkaoui A,et al. Primary epiphyseal or apophyseal subacute osteomyelitis in the pediatric population: a report of fourteen cases and a systematic review of the literature[J]. J Bone Joint Surg Am,2014,96(18):1570-1575.
[3] 施莺燕,帕米尔,马瑞雪,等.小儿长骨骨髓炎的MRI表现[J].放射学实践,2014,29(8):880-884.
[4] Pandey PK,Pawar I,Gupta J. Physeal separation and complete resorption of femoral head associated with chronic osteomyelitis of femoral diaphysis in a young child: rare case report[J]. J Pediatr Orthop B,2016,25(6):529-532.
[5] Goto T,Nemoto T,Ogura K,et al. Eosinophilic granuloma of the capital femoral epiphysis[J]. J Pediatr Orthop B,2011,20(3):157-161.
[6] Newquist JM,Baxter GM. Evaluation of plasma fibrinogen concentration as an indicator of physeal or epiphyseal osteomyelitis in foals:17 cases(2002-2007)[J]. J Am Vet Med Assoc,2009,235(4):415-419.
[7] Mellado Santos JM. Diagnostic imaging of pediatric hematogenous osteomyelitis:lessons learned from a multi-modality approach[J]. Eur Radiol,2006,16(9):2109-2119.
[8] Gilbertson-Dahdal D,Wright JE,Krupinski E. Transphyseal involvement of pyogenic osteomyelitis is considerably more common than classically taught[J]. AJR Am J Roentgenol,2014,203(1):190-195.
[9] Song KM,Boatright KC,Drassler J,et a1. The use of polymerase chain reaction for the detection and speciation of bacterial bone and joint infection in children[J]. J Pediatr Orthop,2009,29(2):182-188.
[10] Kao HK,YangWE,Shih HN,et al. Physeal change after tuberculous osteomyelitis of the long hone in children[J]. Chang Gung Med J,2010,33(4):453-460.
[11] Schallert EK,Kan JH,Monsalve J. Metaphyseal osteomyelitis in children: how often does MRI-documented joint effusion or epiphyseal extension of edema indicate coexisting septic arthritis[J]. Pediatr Radiol,2015,45(8):1174-1181.
[12] Shaikh MJ,Rex C,Vignesh R. Slipped distal femoral epiphysis in congenital insensitivity to pain[J]. J Orthop Case Rep,2016,6(2):78-80.
[13] 苏江宁,赵晓勇,许丽霞,等.中西医结合治疗小儿急性骨髓炎165例[J].河北医科大学学报,2009,30(9):966-967.
[14] Agarwal A,Gupta N,Mishra M. Primary epiphyseal and metaepiphyseal tubercular osteomyelitis in children A series of 8 case[J]. Acta Orthop Belg,2016,82(4):797-805.
[15] Gümüstas SA,Cagirmaz T,Orak MM. Cystic tuberculosis osteomyelitis of the distal tibia in infancy[J]. Turk Pediatri Ars,2017,52(1):53-56.
[16] Yoo WJ,Choi IH,Yun YH,et al. Primary epiphyseal osteomyelitis caused by mycobacterium species in otherwise healthy toddlers[J]. J Bone Joint Surg Am,2014,96(17):e145.