心脏瓣膜病进行性发展至严重阶段多需要行瓣膜置换手术,心脏手术后急性肾损伤(acute kidney injury,AKI)是一个重要的问题。50%患者可能经历肾脏功能减低[血肌酐(serum creatinine,SCr)增加25%],5%需要肾脏替代治疗。AKI术前危险因素包括已有肾功能不全、年龄、糖尿病、吸烟和近期冠状动脉造影。术中危险因素包括体外循环、主动脉阻断时间长和低血压/不良肾灌注。AKI也可以发生在术后,持续血流动力学不稳定会损害肾脏灌注,正性肌力药物应用也与AKI相关。其中最重要的因素之一就是术中需要应用体外循环技术,而体外循环所带来的不良反应之一就是全身炎性反应,情况严重的话,患者术后出现多器官功能不全综合征。AKI甚至肾衰竭发生率很高,作为严重并发症之一,对患者的预后产生不良影响,甚至导致死亡。有研究发现,非体外循环冠状动脉搭桥术后,AKI发生率高达37.1%,AKI组机械通气时间、重症监护病房滞留时间、气管插管复插率、消化道出血发生率、输血量、肾脏替代治疗发生率均高于非AKI组[1]。在一项经历了心脏手术的3 008例患者随访中,AKI发生率为29.1%,从AKI发生到肾脏疾病终末期大约需要5年时间[2]。在针对2 575例经历体外循环心脏手术患者的回顾性分析中,AKI发生率更是高达36%,甚至1.2%患者需要肾脏替代治疗[3]。心脏术后AKI会增加围术期病死率,延长住院时间,增加住院费用[4]。对于AKI 的早期预测和诊断,其指标的滞后是急性肾衰竭病死率居高不下的一个重要原因,故寻找能够早期诊断AKI 的生物学标志物就显得十分重要。既往文献报道,血清中性粒细胞明胶酶相关脂质运载蛋白(neutrophil gelatinase-associated lipocalin,NGAL)和胱抑素C(cystatin C,Cys C)可能对AKI 具有早期诊断作用[5-8]。有研究发现,肾损伤糖尿病儿童中Cys C明显增高,Cys C与糖化血红蛋白(hemoglobin A1c,HbA1c)联合检测在诊断肾损伤方面,其敏感度和特异度均优于单独检测Cys C或HbA1c[9]。还有研究发现,1,2,3期AKI患者血清NGAL显著高于对照组,AKI患者血清NGAL与SCr呈正相关,血清NGAL可作为AKI发生的血清学指标,对AKI的早期诊断具有重要作用[10]。但NGAL和Cys C在瓣膜病术后并发AKI中的诊断作用并不明确。本研究旨在探讨血清NGAL 和Cys C对瓣膜病术后并发AKI的早期诊断价值。
1 资料与方法
1.1 一般资料 选择2018年1—12月河北医科大学第二医院收治的心脏瓣膜病行换瓣手术患者90例。排除标准:①术前已经存在肾功能不全者;②术前或研究期间使用过肾毒性药物者;③术前生命体征不稳定者;④糖尿病及高血压病患者。换瓣手术术中均采用膜肺进行体外循环。按AKI 的诊断标准,发生AKI者37例为AKI 组,未发生AKI者53例为非AKI 组。2组性别、年龄及术前血糖、尿素氮、SCr差异均无统计学意义(P>0.05),具有可比性。
本研究经医院医学伦理委员会批准通过;所有患者均签署知情同意书。
1.2 AKI的诊断标准 根据2012 年改善全球肾脏病预后组织(Kidney Disease Improving Global Outcomes,KDIGO) 的AKI诊断标准: 48 h内SCr增高≥26.5 μmol/L;或SCr增高至≥基础值的1.5倍,且明确或经推断其发生在7 d之内;或持续6 h尿量<0.5 mL·kg-1·h-1[11]。
表1 2组一般资料比较
Table 1 Comparison of general information between two groups![]()
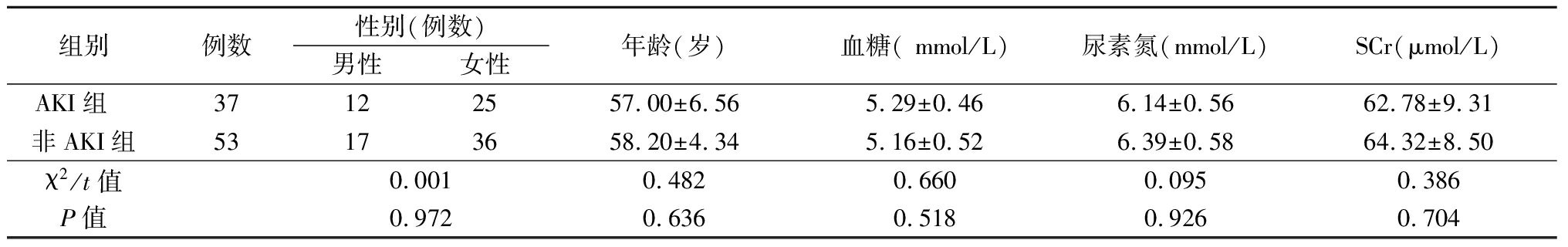
组别例数性别(例数)男性女性年龄(岁)血糖( mmol/L)尿素氮(mmol/L)SCr(μmol/L)AKI组 37122557.00±6.565.29±0.466.14±0.5662.78±9.31非AKI组53173658.20±4.345.16±0.526.39±0.5864.32±8.50χ2/t值0.0010.4820.6600.0950.386P值0.9720.6360.5180.9260.704
1.3 样本采集 所有患者于术前和术后2,4,6,8,12,24,48 h收集血标本,15 min 内离心(2 000 r/min),清除颗粒和聚合物。取血清分成3份,每份1 mL,储存于-20 ℃冰箱备用。
1.4 血清NGAL 测定 采用固相夹心酶联免疫吸附测定法,试剂盒购自美国R&D公司,实验操作严格按说明书进行,试剂盒敏感度为1.0 μg/L,板内、板间变异系数均小于10%。
1.5 SCr测定 采用肌氨酸氧化酶法,试剂盒购自奥林巴斯试剂,仪器应用奥林巴斯AU2700 型全自动生化分析仪,实验操作严格按照说明书进行,浓度单位为μmol/L。
1.6 血清Cys C 测定 采用免疫投射比浊法,试剂盒由宁波美康生物科技有限公司提供,仪器应用奥林巴斯AU2700 型全自动生化分析仪,实验操作严格按照说明书进行。
1.7 统计学方法 应用SPSS 19.0统计软件分析数据。计量资料比较分别采用两独立样本的t检验和重复测量的方差分析,计数资料比较采用χ2检验。P<0.05为差异有统计学意义。
2 结 果
2.1 2组不同时点SCr水平比较 2组SCr水平均呈先升高再降低趋势,AKI组SCr水平变化幅度大于非AKI组,AKI 组肌酐术后12 h明显升高,其组间、时点间、组间·时点间交互作用差异均有统计学意义(P<0.05),见表2。
2.2 2组不同时点血NGAL水平比较 AKI 组血NGAL水平均呈先升高再降低趋势,非AKI组血NGAL水平逐渐降低,AKI组术后2 h血清NGAL明显升高,其组间、时点间、组间·时点间交互作用差异均有统计学意义(P<0.05),见表3。
2.3 2组不同时点血Cys C水平比较 2组血Cys C水平呈逐渐升高趋势,AKI 组血Cys C水平变化幅度大于非AKI组,AKI 组术后6 h明显升高,其组间、时点间、组间·时点间交互作用差异均有统计学意义(P<0.05),见表4。
表2 2组不同时点SCr水平比较
Table 2 Comparison of SCr levels at different time points between two groups![]()
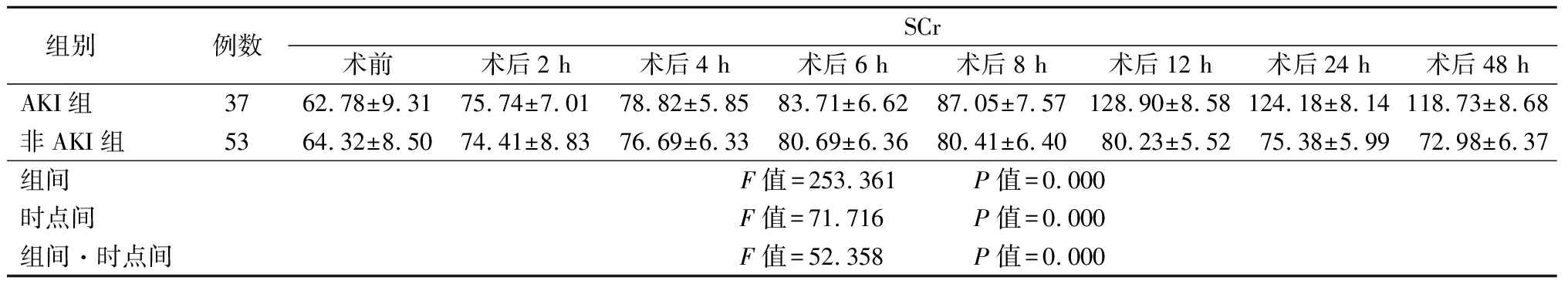
组别例数SCr术前 术后2 h术后4 h术后6 h术后8 h术后12 h术后24 h术后48 hAKI组3762.78±9.3175.74±7.0178.82±5.8583.71±6.6287.05±7.57128.90±8.58124.18±8.14118.73±8.68非AKI组5364.32±8.5074.41±8.8376.69±6.3380.69±6.3680.41±6.4080.23±5.5275.38±5.9972.98±6.37组间F值=253.361 P值=0.000时点间F值=71.716 P值=0.000组间·时点间F值=52.358 P值=0.000
表3 2组不同时点血NGAL 水平比较
Table 3 Comparison of NGAL levels at different time points between two groups![]()
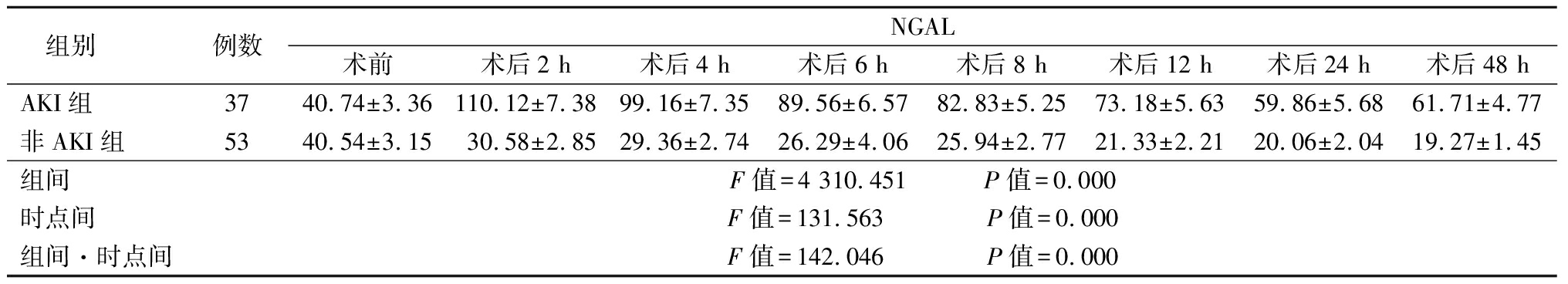
组别例数NGAL术前 术后2 h术后4 h术后6 h术后8 h术后12 h术后24 h术后48 hAKI组3740.74±3.36110.12±7.3899.16±7.3589.56±6.5782.83±5.2573.18±5.6359.86±5.6861.71±4.77非AKI组5340.54±3.1530.58±2.8529.36±2.7426.29±4.0625.94±2.7721.33±2.2120.06±2.0419.27±1.45组间F值=4 310.451 P值=0.000时点间F值=131.563 P值=0.000组间·时点间F值=142.046 P值=0.000
表4 2组不同时点血Cys C水平比较
Table 4 Comparison of Cys C levels at different time points between the two groups![]()
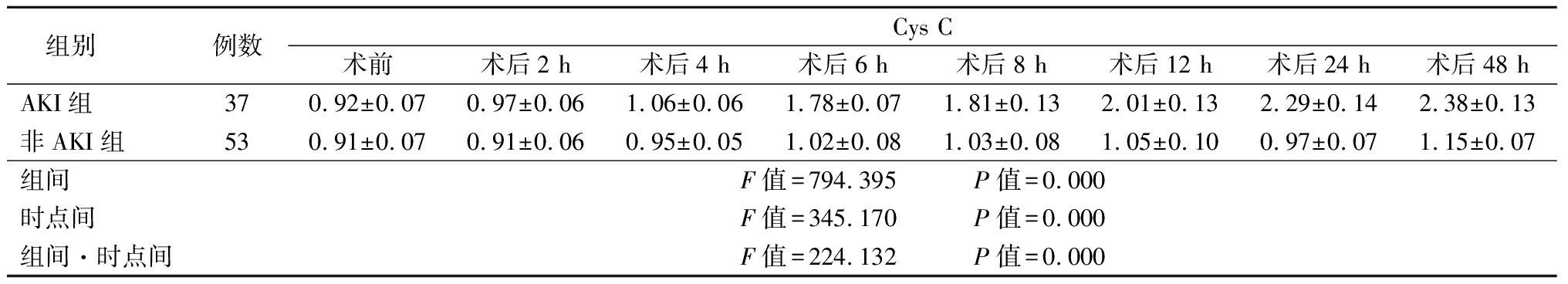
组别例数Cys C术前 术后2 h术后4 h术后6 h术后8 h术后12 h术后24 h术后48 hAKI组370.92±0.070.97±0.061.06±0.061.78±0.071.81±0.132.01±0.132.29±0.142.38±0.13非AKI组530.91±0.070.91±0.060.95±0.051.02±0.081.03±0.081.05±0.100.97±0.071.15±0.07组间F值=794.395 P值=0.000时点间F值=345.170 P值=0.000组间·时点间F值=224.132 P值=0.000
3 讨 论
瓣膜病患者因术中需要体外循环,术后出现系统性炎症反应,导致多器官功能不全,如急性呼吸窘迫综合征[12],加之心肌顿抑,循环不稳,在肾脏方面会出现AKI。二尖瓣置换术后AKI发生率达38.7%[13]。本研究瓣膜病术后发生AKI 37例,发生率为41.1%。对于肾损伤的诊断,一直应用SCr和尿量评价,而心脏术后多需要应用利尿剂对尿量进行干预以达到容量控制,故尿量不是很好的诊断肾损伤的指标。而SCr需要等到肾小球滤过率降低50%以上才出现升高,且要等到肾功能降低到一个比较稳定的程度时SCr才能正确地反映肾脏状况,故SCr反映肾功能损伤比较滞后。本研究AKI组SCr升高峰值出现在术后12~48 h,如果依据SCr水平,需要等到换瓣术后12~48 h才可以作出诊断。但是对于重症患者,对各器官功能损伤的诊断需要尽可能早,以便尽早干预,防止出现器官功能衰竭。因此,寻找AKI的早期诊断指标非常必要。
NGAL是脂质运载蛋白家族的新成员,是在人中性粒细胞中被发现的[14]。NGAL除了在中性粒细胞表达外,还在肾近曲小管细胞、小肠潘氏细胞、肝胆管细胞、胃壁细胞等中表达。肾小管上皮细胞损伤后,尿NGAL升高。有研究显示,AKI早产儿尿NGAL与第2天SCr水平具有明显的相关性,故尿NGAL可以作为早产儿AKI非侵入性的诊断指标[15]。NGAL不仅存在于尿液中,同样也存在于血浆中,血浆中NGAL浓度的测定对AKI的早期诊断将更加有利,因为如果患者尿少,又或者使用利尿剂,均会影响尿中NGAL的检测。有研究显示,经历体外循环后的AKI患者心脏术后2 h血NGAL浓度中即可明显升高[16]。多变量分析显示,血NGAL是急性肾盂肾炎的独立预测因子,优于降钙素原、C反应蛋白、白细胞等[17]。本研究结果显示,换瓣术后AKI组术后血NGAL 水平明显高于非AKI 组,术后2 h为峰值。表明血NGAL是换瓣术后AKI的早期标志物之一。
Cys C 是一种内源性小分子蛋白质,相对分子质量为13 000,是胱蛋白抑制剂家族的一员。Cys C 的生成速度稳定,肾脏是其唯一的排泄器官,且目前认为Cys C不受年龄、饮食和炎症等因素影响,在肾功能损害早期比SCr更敏感,故是早期反映肾小球滤过功能受损的理想指标[18]。荟萃分析包含30个前瞻性研究(包括来自15个国家的4 247例成年人,其中982例患者发生AKI),对于各种原因引起的AKI,Cys C显示出强有力的预测性,受试者工作曲线下面积为0.89,其敏感度和特异度均为0.82[19]。在一项发生AKI的重症患儿调查中显示,血浆Cys C在患儿入重症监护病房12 h明显升高,早于SCr水平的升高[20]。对危重患者分别应用RIFLE、AKI网络工作小组、KDIGO和 Cys C标准进行AKI诊断和预后分析,发现Cys C对重症AKI患者的短期结果比其他3项有更高的预测性[21]。本研究结果显示,AKI 患者Cys C水平在SCr升高之前(术后6 h)就已明显升高。表明Cys C诊断AKI的敏感度可能高于SCr,提示血Cys C是换瓣术后AKI的早期标志物之一。
总之,换瓣术后检测NGAL、Cys C水平有助于早期诊断AKI的发生,可为尽早干预提供有效证据,NGAL、Cys C检测稳定、可靠、价格便宜且容易操作,故应用前景优势明显。
[1] Li XH,Xiao F,Zhang SY. Investigation of risk factors of acute kidney injury after off-pump coronary artery bypass grafting and 3 years follow-up[J]. Beijing Da Xue Xue Bao,2017,49(1):131-136.
[2] Chew ST,Ng RR,Liu W,et al. Acute kidney injury increases the risk of end-stage renal disease after cardiac surgery in an Asian population: a prospective cohort study[J]. BMC Nephrol,2017,18(1):60.
[3] Xie X,Wan X,Ji X,et al. Reassessment of acute kidney injury after cardiac surgery:a retrospective study[J]. Intern Med,2017,56(3):275-282.
[4] Sawhney S,Fraser SD. Epidemiology of AKI:utilizing large databases to determine the burden of AKI[J]. Adv Chronic Kidney Dis,2017,24(4):194-204.
[5] Introcaso G,Nafi M,Bonomi A,et al. Improvement of neutrophil gelatinase-associated lipocalin sensitivity and specificity by two plasma measurements in predicting acute kidney injury after cardiac surgery[J]. Biochem Med(Zagreb),2018,28(3):030701.
[6] Kanchi M,Manjunath R,Massen J,et al. Neutrophil gelatinase-associated lipocalin as a biomarker for predicting acute kidney injury during off-pump coronary artery bypass grafting[J]. Ann Card Anaesth,2017,20(3):297-302.
[7] Tecson KM,Erhardtsen E,Eriksen PM,et al. Optimal cut points of plasma and urine neutrophil gelatinase-associated lipocalin for the prediction of acute kidney injury among critically ill adults:retrospective determination and clinical validation of a prospective multicentre study[J]. BMJ Open,2017,7(7):e016028.
[8] Ebru AE,Kilic A,Korkmaz FS,et al. Is cystatin-C superior to creatinine in the early diagnosis of contrast-induced nephropathy?:a potential new biomarker for an old complication[J]. J Postgrad Med,2014,60(2):135-140.
[9] Qian T,Tian L,Li Y,et al. Value of the combined examination of Cys-C and HbA1c for diagnosis of early renal injury in pediatric diabetes[J]. Exp Ther Med,2017,13(2):515-518.
[10] 赵帅,耿玉兰,代丽丽,等.血清中性粒细胞明胶酶相关脂质运载蛋白检测诊断急性肾损伤的临床价值[J].河北医科大学学报,2013,34(4):416-417.
[11] Khwaja A. KDIGO clinical practise guideline for acute kidney injury[J]. Nephron Clin Pract,2012,120(4):c179-184.
[12] 王立孟.体外循环瓣膜置换术后ALI/ARDS的临床研究[J].河北医科大学学报,2012,33(6):684-685.
[13] Chang CH,Lee CC,Chen SW,et al. Predicting acute kidney injury following mitral valve repair[J]. Int J Med Sci,2016,13(1):19-24.
[14] Kjeldsen L,Johnsen AH,Sengelov H,et al. Isolation and primary stueture of NGAL,a novel protein associated withneutrophil gelatinase[J]. J Biol Chem,1993,268(14):10425-10432.
[15] Kuribayashi R,Suzumura H,Sairenchi T,et al. Urinary neutrophil gelatinase-associated lipocalin is an early predictor of acute kidney injury in premature infants[J]. Exp Ther Med,2016,12(6):3706-3710.
[16] Kalisnik JM,Hrovat E,Hrastovec A,et al. Creatinine,neutrophil gelatinase-associated lipocalin,and cystatin c in determining acute kidney injury after heart operations using cardiopulmonary bypass[J]. Artif Organs,2017,41(5):481-489.
[17] Kim BK,Yim HE,Yoo KH. Plasma neutrophil gelatinase-associated lipocalin: a marker of acute pyelonephritis in children[J]. Pediatr Nephrol,2017,32(3):477-484.
[18] Hassinger AB,Backer CL,Lane JC,et al. Predictive power of serum cystatin C to detect acute kidney injury and pediatric-modified RIFLE class in children undergoing cardiac surgery[J]. Pediatr Crit Care Med,2012,13(4):435-440.
[19] Yong Z,Pei X,Zhu B,et al. Predictive value of serum cystatin C for acute kidney injury in adults: a meta-analysis of prospective cohort trials[J]. Sci Rep,2017,7:41012.
[20] Safdar OY,Shalaby M,Khathlan N,et al. Serum cystatin is a useful marker for the diagnosis of acute kidney injury in critically ill children: prospective cohort study[J]. BMC Nephrol,2016,17(1):130.
[21] Zhou J,Liu Y,Tang Y,et al. A comparison of RIFLE,AKIN,KDIGO,and Cys-C criteria for the definition of acute kidney injury in critically ill patients[J]. Int Urol Nephrol,2016,48(1):125-132.