沙滩椅体位维持了人体肩与上臂的自然体位关系,便于肩关节相关骨科手术的复位及操作等,被广泛应用[1]。然而,术中特殊体位的维持可导致外周神经损伤。既往研究报道患者处于沙滩椅体位时,外周神经损伤的发生率为0.6%~81%[2]。股外侧皮神经(lateral femoral cutaneous nerve,LFCN)是由腰2、腰3神经根发出的在腰大肌外缘汇成一支斜向外下走行的粗大神经,股外侧皮神经麻痹(lateral femoral cutaneous nerve palsy,LFCNP)是沙滩椅体位常见的外周神经损伤并发症,可导致股外侧皮肤部位感觉及痛觉敏感,随着病情的发展可转化为皮神经麻痹,其痛觉、温觉、触觉退钝或消失[3]。多数患者在6个月内自行缓解,但部分患者缓解期可达2年以上[4]。本研究回顾性分析河北省沧州市中心医院在沙滩椅体位下行肩关节镜手术治疗患者的临床资料,探讨该类患者术后LFCNP的危险因素,旨在为提高临床医疗安全提供依据和指导。
1 资料与方法
1.1 一般资料 回顾性分析2014 年1月1日—2017 年12月31日于河北省沧州市中心医院在沙滩椅体位下行肩关节镜手术治疗的254例患者的临床资料,临床资料来源于临床病历系统(Mandala,无锡)和手术室麻醉记录系统(Docare,苏州)。纳入标准:①沙滩椅体位下行肩关节镜手术治疗;②无精神性疾病。排除标准:①临床资料不完整;②腰椎相关疾病导致的下肢放射性疼痛;③术前存在LFCNP。根据患者术后是否发生LFCNP分为LFCNP组8例和非LFCNP组246例。
1.2 沙滩椅体位摆放 待患者麻醉满意后,将手术床调节为沙滩椅样,患者仰卧位髋部屈曲90~110 °,膝部屈曲20~30 °。根据病情需要将手术台上1/3部分置头高45 °,中1/3部置头低45 °,下1/3部置脚低10~15 °。患者坐于手术台中1/3交界处,小止腿位于手术台下1/3处。防头部左右摇摆,2根约束带分别将头和下颌固定牢固,保持头屈曲位以便颈后部伸直,保持下颌与胸骨2~3 cm。防止脊髓缺血损伤。脚下放置挡脚板,防止身体下滑移位。床头或术侧肩胛后垫1个5~8 cm的小枕,用中单包裹膝枕垫垫在膝下,将中单两端的带子固定于手术床缘上避免患者下滑。
1.3 观察指标 所有患者在麻醉诱导前均接受标准的术中监护,包括无创动脉压力监测、脉氧饱和度、5导联心电监测、体表温度监测。记录患者的人口学资料(性别、年龄、身高、体重)、美国麻醉医师协会(American Society of Anesthesiologists,ASA)、体重指数(body mass index, BMI)、术前合并症(高血压史、2型糖尿病史);记录麻醉方法(全身麻醉或局部麻醉)、围术期输液量、尿量、出血量、手术时间。记录患者术后24 h内股外侧是否存在疼痛、麻木症状,若存在以上症状则被诊断为LFCNP,并进行跟踪随访。
1.4 统计学方法 应用SPSS 18.0统计软件分析数据。计量资料以中位数(四分位数间距)表示,组间比较采用秩和检验;计数资料比较采用χ2检验;危险因素确定采用二元Logistic回归分析。P<0.05为差异有统计学意义。
2 结 果
2.1 2组人口统计学指标比较 LFCNP组BMI明显高于非LFCNP组,差异有统计学意义(P<0.05);2组性别、年龄、身高、体重、ASA分级、术前并发症(高血压史、2型糖尿病史)差异均无统计学意义(P>0.05)。见表1。
表1 2组人口统计学指标比较
Table 1 Comparison of demographic index between two groups
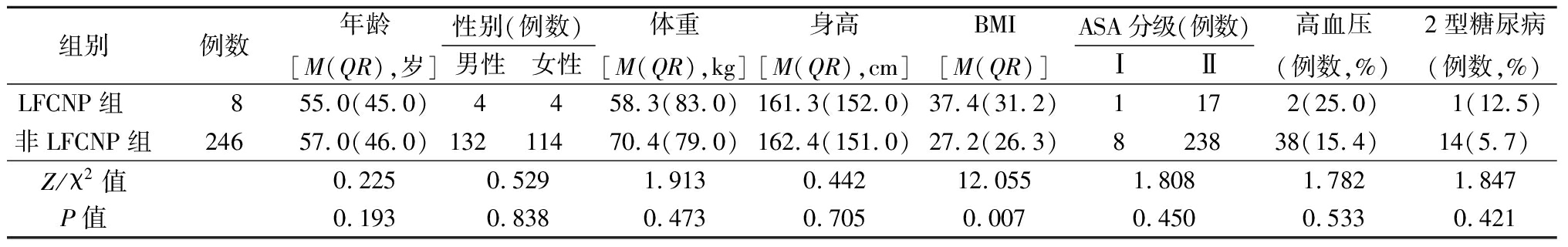
组别例数年龄[M(QR),岁]性别(例数)男性女性体重[M(QR),kg]身高[M(QR),cm]BMI[M(QR)]ASA分级(例数)ⅠⅡ高血压(例数,%)2型糖尿病(例数,%)LFCNP组 855.0(45.0)4458.3(83.0)161.3(152.0)37.4(31.2)1172(25.0) 1(12.5)非LFCNP组24657.0(46.0)13211470.4(79.0)162.4(151.0)27.2(26.3)823838(15.4)14(5.7)Z/χ2值0.2250.5291.9130.44212.0551.8081.7821.847P值0.1930.8380.4730.7050.0070.4500.5330.421
2.2 2组围术期指标比较 LFCNP组手术时间明显长于非LFCNP组,差异有统计学意义(P<0.05);2组麻醉方法、输注液量、尿量、失血量差异均无统计学意义(P>0.05)。见表2。
表2 2组围术期指标比较
Table 2 Comparison of peri-operative index between two groups
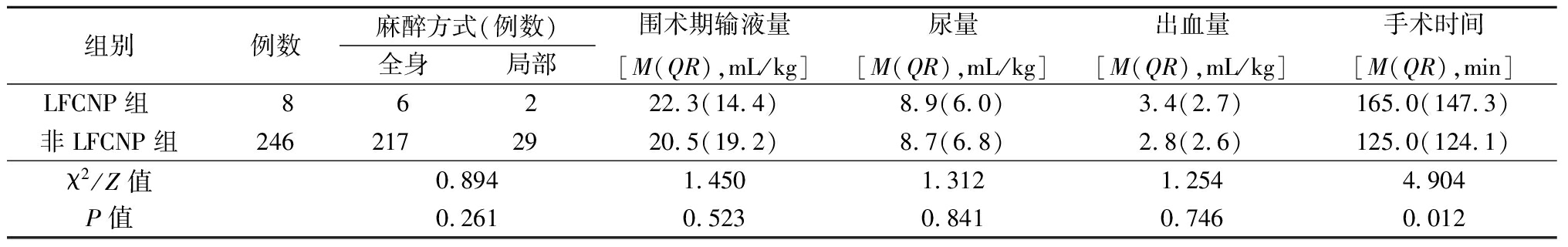
组别例数麻醉方式(例数)全身局部围术期输液量[M(QR),mL/kg]尿量[M(QR),mL/kg]出血量[M(QR),mL/kg]手术时间[M(QR),min]LFCNP组 86222.3(14.4)8.9(6.0)3.4(2.7)165.0(147.3)非LFCNP组2462172920.5(19.2)8.7(6.8)2.8(2.6)125.0(124.1)χ2/Z值0.8941.4501.3121.2544.904P值0.2610.5230.8410.7460.012
2.3 二元Logistic回归分析 以术后发生LFCNP(发生=1,未发生=0)为自变量,以BMI>28(是=1,否=0)、手术时间>2 h(是=1,否=0)为因变量,进行二元Logistic 回归分析,结果显示BMI>28和手术时间>2 h是患者术后发生LFCNP的危险因素,见表3。
表3 术后LFCNP的危险因素分析
Table 3 The analysis of risk factors in patients with post-operative LFCNP
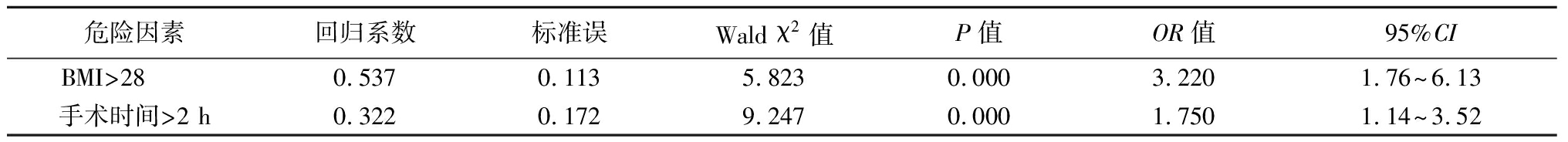
危险因素回归系数标准误Wald χ2值P值OR值95%CIBMI>28 0.5370.1135.8230.0003.2201.76~6.13手术时间>2 h0.3220.1729.2470.0001.7501.14~3.52
3 讨 论
围术期体位摆放和变动过程中,着力点不当,可导致神经承受的组织压力及牵引力增加,一旦超过其所承受的物理限度,可造成术后严重神经损伤[5-6];同时,由于术中体位的牵拉、周围相关组织的压迫,可造成神经缺血,易诱发体位性神经损伤[7]。既往研究表明,体位性神经损伤的严重程度与神经受力面积及周围组织对神经的压强有关[8]。股外侧脂肪组织较少,股外侧皮神经易受沙滩体位下外界压迫和牵拉,造成术后LFCNP[9]。因此,如何减少沙滩椅体位下肩关节术后LFCNP,识别造成体位相关性神经损伤的围术期危险因素是当前的重要任务。
Juhl等[10]在一项包含了252例行胸腰段脊柱手术患者的队列研究中发现,术后神经麻痹的发生与患者BMI增加相关。Parisi等[11]报道,即使在排除了性别和年龄等因素干扰后,术后发生LFCNP患者的平均BMI显著仍高于非LFCNP患者。另有研究发现,即使是未行手术治疗,肥胖患者发生LFCNP的概率仍明显高于正常人[12]。本研究结果发现,BMI>28是沙滩椅体位下行肩关节手术后发生LFCNP的危险因素。至今为止,BMI升高导致术后LFCNP发生率增加的具体机制尚未阐明,沙滩位导致腹部弯曲、腹股沟韧带前移、髂筋膜压力增加,加之肥胖患者腹部膨胀,脂肪和内脏重量增加,均可增加股外侧皮神经周围组织的压力[9,13]。有研究表明,坐位下肥胖最大可增加股外侧皮神经周围组织50 mmHg(1 mmHg=0.133 kPa)的压力,围术期股外侧皮神经周围压力的增加,可能是沙滩椅体位下术后发生LFCNP的主要原因[14]。
手术时间延长是围术期发生体位性神经损伤的危险因素,其机制可能与体位压迫和牵拉,造成神经压力升高,周围血液供应减少相关[15]。既往文献报道,手术时间延长可能是术后发生LFCNP的相关危险因素[4]。本研究结果显示,LFCNP组手术时间明显长于非LFCNP组,且手术时间>2 h是沙滩椅体位下术后发生LFCNP的危险因素。因此,应尽可能地缩短手术时间,这对于存在术后LFCNP高危险因素的患者(如BMI>28)是避免发生体位相关性神经损伤的主要防治措施[16-17]。
糖尿病可增加坐位术后感觉异常性股痛发生率,其机制可能与长期血糖控制不佳导致神经对压迫造成缺氧敏感性升高有关[18-19]。长期糖类代谢紊乱,血管周围渗透压发生改变,造成糖基化终末产物的形成,神经微血管生长及营养供应发生改变,自身免疫和氧化应激对神经本身产生攻击效应,致使神经生长因子长期供应不足,以上多种因素可导致神经轴索在传递神经冲动过程中发生各种改变,造成感觉异常[20-21]。但部分研究表明,进行了倾向性匹配后,排除了年龄、体重等干扰因素后,糖尿病不再是术后神经麻痹的相关危险因素[10]。本研究结果显示,LFCNP组与非LFCNP组糖尿病发生率差异无统计学意义。可能与围术期麻醉医生对轴索血糖等内环境优化后,避免了糖尿病可能对神经轴索造成的损伤有关。
全身麻醉是否对术后患者外周神经损伤的发生率造成影响一直是近年来研究的热点[22]。由于全身麻醉后,患者本身意识丧失,导致自我保护功能丧失,不能对体位不当造成的压迫和牵拉作出保护性反应[23];同时,全身麻醉后导致血管扩张,全身血流动力学发生剧烈变化,造成外周灌注不足,导致周围神经发生缺血再灌注损伤,也可能是全身麻醉导致外周神经损伤发生率升高的原因[24]。本研究结果显示,LFCNP组与非LFCNP组全身麻醉和局部麻醉差异无统计学意义。在既往研究中也显示全身麻醉不会增加体位相关神经损伤的发生率[12]。这可能与护理人员在体位摆放过程中尽量避免人为性压迫和牵拉、术中血流动力学稳定有关。
综上所述,BMI>28、手术时间>2 h是沙滩椅体位下肩关节术后LFCNP的危险因素。但本研究为回顾性研究,其结论尚需要大样本前瞻性研究进一步证实。
[1] Li X,Eichinger JK,Hartshorn T,et al. A comparison of the lateral decubitus and beach-chair positions for shoulder surgery:advantages and complications[J]. J Am Acad Orthop Surg,2015,23(1):18-28.
[2] Chiaghana CO,Awoniyi CA. Delayed onset and long-lasting hemidiaphragmatic paralysis and cranial nerve deficit after interscalene nerve block for rotator cuff repair in beach chair position[J]. J Clin Anesth,2016,34:571-576.
[3] Levy BJ,Tauberg BM,Holtzman AJ,et al. Reducing lateral femoral cutaneous nerve palsy in obese patients in the beach chair position:effect of a standardized positioning and padding protocol[J]. J Am Acad Orthop Surg,2018[Epub ahead of print].
[4] Holtzman AJ,Glezos CD,Feit EJ,et al. Prevalence and risk factors for lateral femoral cutaneous nerve palsy in the beach chair position[J]. Arthroscopy,2017,33(11):1958-1962.
[5] Abdalmageed OS,Bedaiwy MA,Falcone T. Nerve injuries in gynecologic laparoscopy[J]. J Minim Invasive Gynecol,2017,24(1):16-27.
[6] Duffy BJ,Tubog TD. The prevention and recognition of ulnar nerve and brachial plexus injuries[J]. J Perianesth Nurs,2017,32(6):636-649.
[7] Le Bocq C,Rousseaux M,Buisset N,et al. Effects of tibial nerve neurotomy on posture and gait in stroke patients:a focus on patient-perceived benefits in daily life[J]. J Neurol Sci,2016,366:158-163.
[8] Hewson DW,Bedforth NM,Hardman JG. Peripheral nerve injury arising in anaesthesia practice[J]. Anaesthesia,2018,73(Suppl 1):51-60.
[9] Sanders AE,Andras LM,Choi PD,et al. Lateral femoral cutaneous nerve palsy after spinal fusion for Adolescent Idiopathic Scoliosis(AIS)[J]. Spine(Phila Pa 1976),2016,41(19):E1164-1167.
[10] Juhl CS,Ballegaard M,Bestle MH,et al. Meralgia paresthetica after prone positioning ventilation in the intensive care unit[J]. Case Rep Crit Care,2016,2016:7263201.
[11] Parisi TJ,Mandrekar J,Dyck PJ,et al. Meralgia paresthetica relation to obesity,advanced age,and diabetes mellitus[J]. Neurology,2011,77(16):1538-1542.
[12] Satin AM,DePalma AA,Cuellar J,et al. Lateral femoral cutaneous nerve palsy following shoulder surgery in the beach chair position:a report of 4 cases[J]. Am J Orthop(Belle Mead NJ),2014,43(9):E206-209.
[13] Sang W,Zhu L,Ma J,et al. The Influence of body mass index and hip anatomy on direct anterior approach total hip replacement[J]. Med Princ Pract,2016,25(6):555-560.
[14] Weng W,Wei Y,Huang W,et al. Risk factor analysis for meralgia paresthetica:a hospital-based study in Taiwan[J]. J Clin Neurosci,2017,43:192-195.
[15] Devi BI,Konar SK,Bhat DI,et al. Predictors of surgical outcomes of traumatic peripheral nerve injuries in children:an institutional experience[J]. Pediatr Neurosurg,2018,53(2):94-99.
[16] Li J,Zeng H,Li Z,et al. Anesthesia for a parturient with intraneural perineurioma:a case report[J].Medicine(Baltimore),2017,96(49):e9135.
[17] Liu J,Hai Y,Kang N,et al. Risk factors and preventative measures of early and persistent dysphagia after anterior cervical spine surgery:a systematic review[J]. Eur Spine J,2018,27(6):1209-1218.
[18] Chung J. Endovascular devices and revascularization techniques for limb-threatening ischemia in individuals with diabetes[J]. J Diabetes Sci Technol,2017,11(5):904-913.
[19] Chen Q,Chiheb S,Fysekidis M,et al. Arterial stiffness is elevated in normotensive type 2 diabetic patients with peripheral neuropathy[J]. Nutr Metab Cardiovasc Dis,2015,25(11):1041-1049.
[20] Pujia A,Gazzaruso C,Montalcini T. An update on the potential role of C-peptide in diabetes and osteoporosis[J]. Endocrine,2017,58(3):408-412.
[21] 吴志伟,宋朋飞.神经病理性疼痛机制研究进展[J].河北医科大学学报,2018,39(9):1095-1100.
[22] Kamel I,Zhao H,Koch SA,et al. The use of somatosensory evoked potentials to determine the relationship between intraoperative arterial blood pressure and intraoperative upper extremity position-related neurapraxia in the prone surrender position during spine surgery:a retrospective analysis[J]. Anesth Analg,2015,122(5):1423-1433.
[23] Bambaren IA,Dominguez F,Martin ME,et al. Anesthesia and analgesia in the patient with an unstable shoulder[J]. Open Orthop J,2017,11:848-860.
[24] Hewson DW,Bedforth NM,Hardman JG. Spinal cord injury arising in anaesthesia practice[J]. Anaesthesia,2018,73(Suppl):43-50.