肥厚型心肌病(hypertrophic cardiomyopathy,HCM)是最常见的遗传性心血管疾病,发病率为1∶500~1∶200,患者自然病程差异大、临床表现多样,部分无明显症状或症状轻微,也有相当数量的患者出现不明原因的晕厥,给日常生活带来潜在危险,若未予重视或抢救不及时可能导致严重的临床后果[1-3]。目前对HCM的研究多集中于心功能的评估,而患者颈部和颅脑血流动力学情况以及是否与其症状相关尚不清楚。本研究通过比较HCM患者和正常人心脏、颈部和颅脑血管超声相关参数,重点探讨HCM患者颈脑血流动力学变化,旨在为HCM患者全面临床评估、早期治疗和预后判断提供影像学依据,报告如下。
1 资料与方法
1.1 一般资料 选取2017年10月—2019年1月我院肥厚型心肌病诊疗中心就诊的成人HCM患者40例,出现胸痛19例,胸闷22例,心悸10例,气短15例,晕厥14例,家庭猝死史2例,服用血管紧张素转换酶抑制剂/血管紧张素受体拮抗剂8例、β受体阻滞剂15例、钙拮抗剂8例。所有患者进行病史采集、体格检查、心脏超声、颈部血管和颅脑血管彩色多普勒检查。纳入标准:①符合HCM诊断标准[4],临床不能解释的左心室某一节段或多个节段室壁厚度≥15 mm;②年龄≥16岁。排除标准:①严重高血压,血压≥160/100 mmHg(1 mmHg=0.133 kPa)、瓣膜性心脏病、先天性心脏病、代谢性疾病等引起心室肥厚、运动员心室肥厚;②合并严重颈脑血管疾病(颈脑血管畸形与狭窄)及焦虑患者。另外纳入我院体检正常的受检者25例作为对照组。2组性别、年龄、体表面积、体重指数、收缩压、舒张压、心率差异均无统计学意义(P>0.05),具有可比性,见表1。
表1 2组一般资料比较
Table 1 Comparison of clinical data between two groups![]()
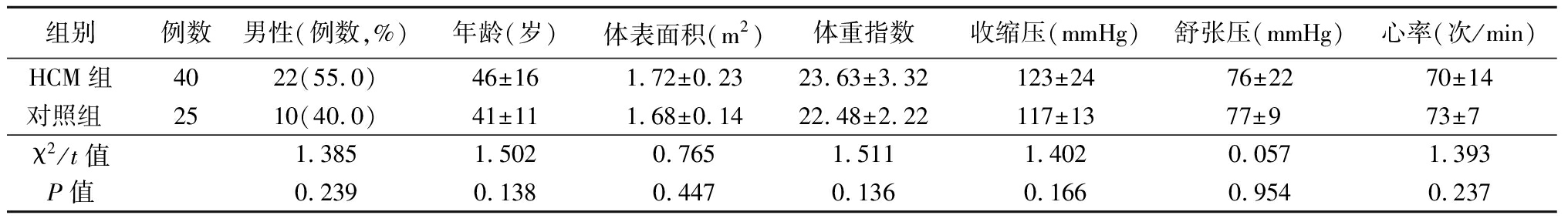
组别例数男性(例数,%)年龄(岁)体表面积(m2)体重指数收缩压(mmHg)舒张压(mmHg)心率(次/min)HCM组4022(55.0)46±161.72±0.2323.63±3.32123±2476±2270±14对照组 2510(40.0)41±111.68±0.1422.48±2.22117±1377±9 73±7 χ2/t值1.3851.5020.7651.5111.4020.0571.393P值0.2390.1380.4470.1360.1660.9540.237
1.2 数据收集
1.2.1 心脏超声与数据测量 应用Philips IE33超声诊断仪,S5-1探头(1~5 MHz)行心脏超声检查。根据指南[5]测量左心室最大室壁厚度(maximal left ventricular wall thickness,MLVWT)、左心室舒张末期内径(left ventricular end-diastolic diameter,LVEDD)、左心室舒张末期容积(left ventricular end-diastolic volume,LVEDV)、左心室收缩末期容积(left ventricular end-systolic volume,LVESV)、左心室射血分数(left ventricular ejection fraction,LVEF)、左心室流出道峰值压力阶差(left ventricular outflow tract pressure gradients,LVOT-PG)、左心房前后径(left atrial diameter,LAD)、二尖瓣口和瓣环舒张早期血流峰速(E峰和e′),计算E/e′比值。
1.2.2 颈部和颅脑血管彩色多普勒超声与数据测量 应用Philips IU Elite超声诊断仪,L9-3探头(3~9 MHz)和S5-1探头(1~5 MHz)。沿胸锁乳头肌水平检查双侧颈总动脉(common carotid artery,CCA)、颈内动脉(internal carotid artery,ICA)和椎动脉(vertebral artery,VA);经颞窗检查双侧大脑中动脉(middle cerebral artery,MCA)、大脑前动脉(anterior cerebral artery,ACA)和大脑后动脉(posterior cerebral artery,PCA);经枕窗检查双侧椎动脉颅内段(vertebral artery-intracranial,VA-IC)和基底动脉(basilar artery,BA)。根据指南[6]测量收缩期最大血流速度(peak systolic velocity,PSV)、舒张末期最大血流速度(maximum end-diastolic velocity,EDV)、舒张末期平均血流速度(average end-diastolic velocity,MDV)、搏动指数(pulsative index,PI)、阻力指数(resistance index,RI)、血流速度时间积分(velocity-time integrals,VTI)、收缩期和舒张期流速比(S/D)和平均血流速度(mean velocity,Mean)。
1.3 统计学方法 应用SPSS 22.0统计软件分析数据。计量资料比较采用两独立样本t检验;计数资料比较采用χ2检验。P<0.05为差异有统计学意义。
2 结 果
2.1 心脏超声比较 HCM组MLVWT、LVOT-PG、LAD、E/e′比值均明显高于对照组(P<0.05);2组其余指标差异均无统计学意义(P>0.05)。见表2。
表2 2组超声心动图指标比较
Table 2 Comparison of echocardiographic parameters between two groups ![]()
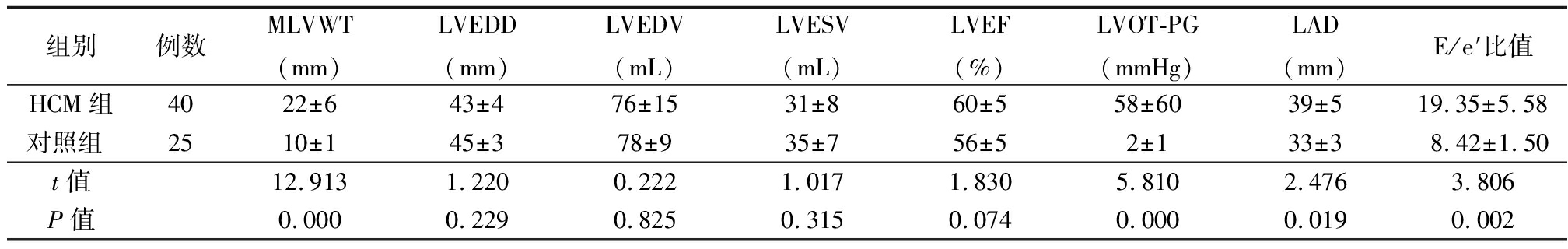
组别例数MLVWT(mm)LVEDD(mm)LVEDV(mL)LVESV(mL)LVEF(%)LVOT-PG(mmHg)LAD(mm)E/e′比值HCM组4022±643±476±1531±860±558±6039±519.35±5.58对照组 2510±145±378±935±756±52±133±38.42±1.50t值12.9131.2200.2221.0171.8305.8102.4763.806P值0.0000.2290.8250.3150.0740.0000.0190.002
2.2 颈部血管超声比较 HCM组双侧CCA的EDV、MDV和VTI均低于对照组,PI和RI均高于对照组(P<0.05);右侧ICA的PSV、EDV、MDV均低于对照组,PI和RI均高于对照组(P<0.05);左侧ICA的EDV低于对照组,PI和RI均高于对照组(P<0.05);右侧VA的PI和RI均高于对照组(P<0.05);左侧VA的EDV低于常对照组,PI和RI均高于对照组(P<0.05);2组其余指标差异均无统计学意义(P>0.05)。见表3。
2.3 颅内血管超声比较 HCM组左侧MCA的RI和Mean均高于对照组(P<0.05);双侧PCA和左侧ACA的VTI均高于对照组(P<0.05);右侧VA-IC的PSV、PI、RI和SD均高于对照组(P<0.05);2组其余颅内血管血流动力学参数差异均无统计学意义(P>0.05)。见表4。
表3 2组颈部血管超声指标比较
Table 3 Comparison of carotid arteries ultrasound between two groups![]()
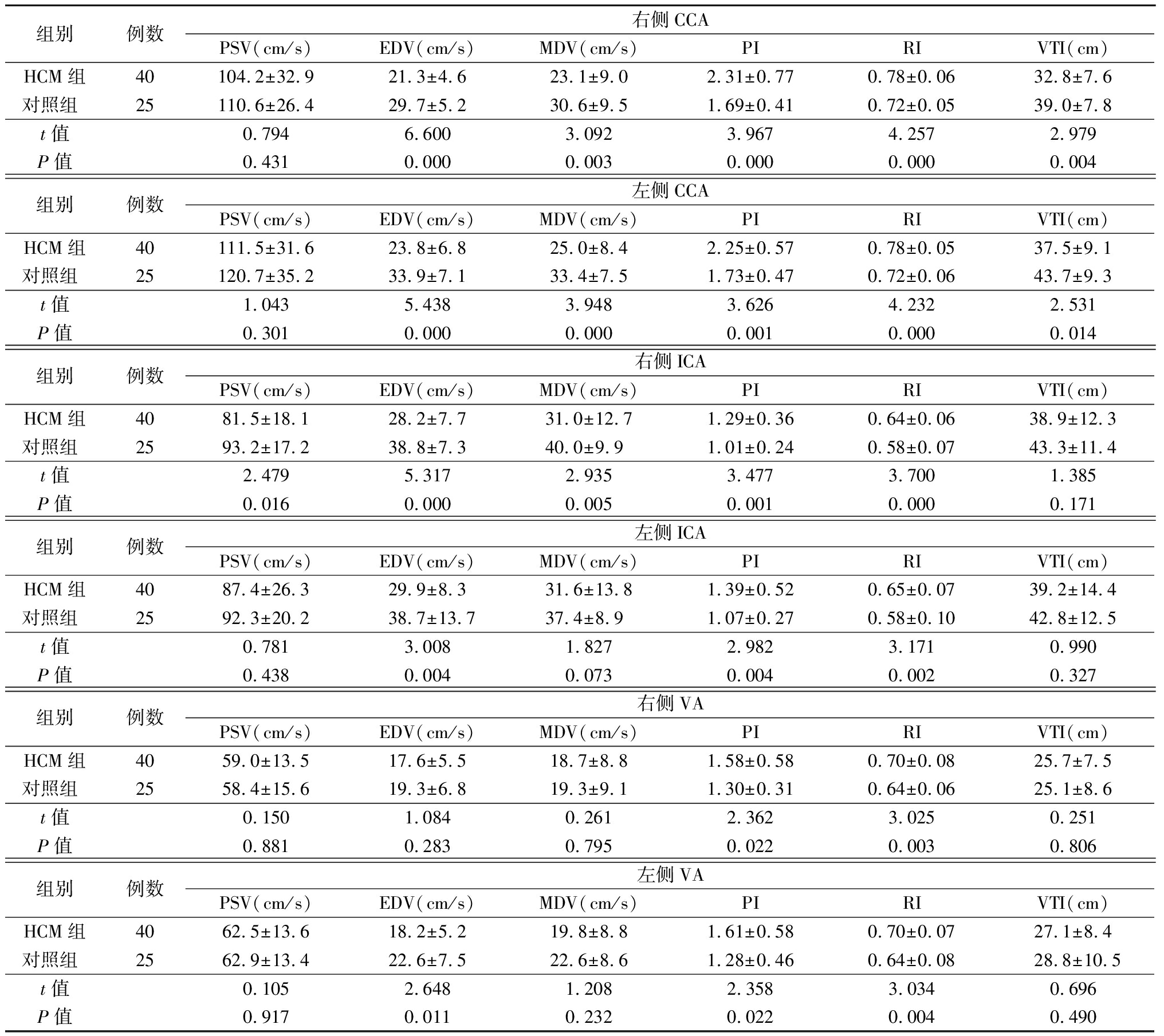
组别例数右侧CCAPSV(cm/s)EDV(cm/s)MDV(cm/s)PIRIVTI(cm)HCM组40104.2±32.921.3±4.623.1±9.02.31±0.770.78±0.0632.8±7.6对照组 25110.6±26.429.7±5.230.6±9.51.69±0.410.72±0.0539.0±7.8t值0.7946.6003.0923.9674.2572.979P值0.4310.0000.0030.0000.0000.004组别例数左侧CCAPSV(cm/s)EDV(cm/s)MDV(cm/s)PIRIVTI(cm)HCM组40111.5±31.623.8±6.825.0±8.42.25±0.570.78±0.0537.5±9.1对照组 25120.7±35.233.9±7.133.4±7.51.73±0.470.72±0.0643.7±9.3t值1.0435.4383.9483.6264.2322.531P值0.3010.0000.0000.0010.0000.014组别例数右侧ICAPSV(cm/s)EDV(cm/s)MDV(cm/s)PIRIVTI(cm)HCM组4081.5±18.128.2±7.731.0±12.71.29±0.360.64±0.0638.9±12.3对照组 2593.2±17.238.8±7.340.0±9.91.01±0.240.58±0.0743.3±11.4t值2.4795.3172.9353.4773.7001.385P值0.0160.0000.0050.0010.0000.171组别例数左侧ICAPSV(cm/s)EDV(cm/s)MDV(cm/s)PIRIVTI(cm)HCM组4087.4±26.329.9±8.331.6±13.81.39±0.520.65±0.0739.2±14.4对照组 2592.3±20.238.7±13.737.4±8.91.07±0.270.58±0.1042.8±12.5t值0.7813.0081.8272.9823.1710.990P值0.4380.0040.0730.0040.0020.327组别例数右侧VAPSV(cm/s)EDV(cm/s)MDV(cm/s)PIRIVTI(cm)HCM组4059.0±13.517.6±5.518.7±8.81.58±0.580.70±0.0825.7±7.5对照组 2558.4±15.619.3±6.819.3±9.11.30±0.310.64±0.0625.1±8.6t值0.1501.0840.2612.3623.0250.251P值0.8810.2830.7950.0220.0030.806组别例数左侧VAPSV(cm/s)EDV(cm/s)MDV(cm/s)PIRIVTI(cm)HCM组4062.5±13.618.2±5.219.8±8.81.61±0.580.70±0.0727.1±8.4对照组 2562.9±13.422.6±7.522.6±8.61.28±0.460.64±0.0828.8±10.5t值0.1052.6481.2082.3583.0340.696P值0.9170.0110.2320.0220.0040.490
表4 2组颅内血管超声指标比较
Table 4 Comparison of cerebral arteries ultrasound between two groups![]()
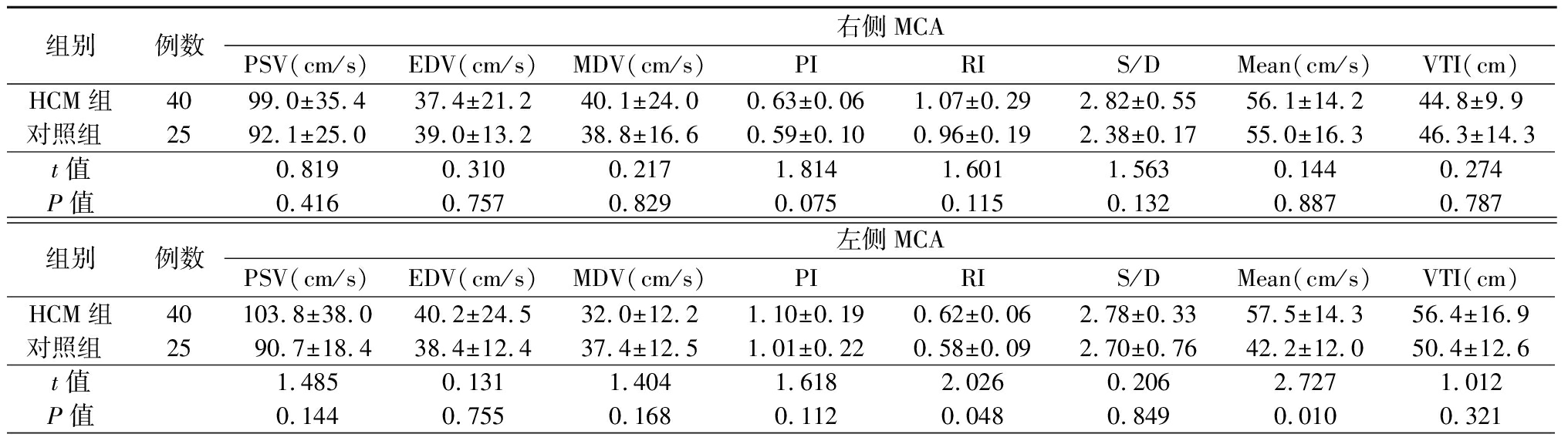
组别例数右侧MCAPSV(cm/s)EDV(cm/s)MDV(cm/s)PIRIS/DMean(cm/s)VTI(cm)HCM组4099.0±35.437.4±21.240.1±24.00.63±0.061.07±0.292.82±0.5556.1±14.244.8±9.9对照组 2592.1±25.039.0±13.238.8±16.60.59±0.100.96±0.192.38±0.1755.0±16.346.3±14.3t值0.8190.3100.2171.8141.6011.5630.1440.274P值0.4160.7570.8290.0750.1150.1320.8870.787组别例数左侧MCAPSV(cm/s)EDV(cm/s)MDV(cm/s)PIRIS/DMean(cm/s)VTI(cm)HCM组40103.8±38.040.2±24.532.0±12.21.10±0.190.62±0.062.78±0.3357.5±14.356.4±16.9对照组 2590.7±18.438.4±12.437.4±12.51.01±0.220.58±0.092.70±0.7642.2±12.050.4±12.6t值1.4850.1311.4041.6182.0260.2062.7271.012P值0.1440.7550.1680.1120.0480.8490.0100.321
表4 (续)
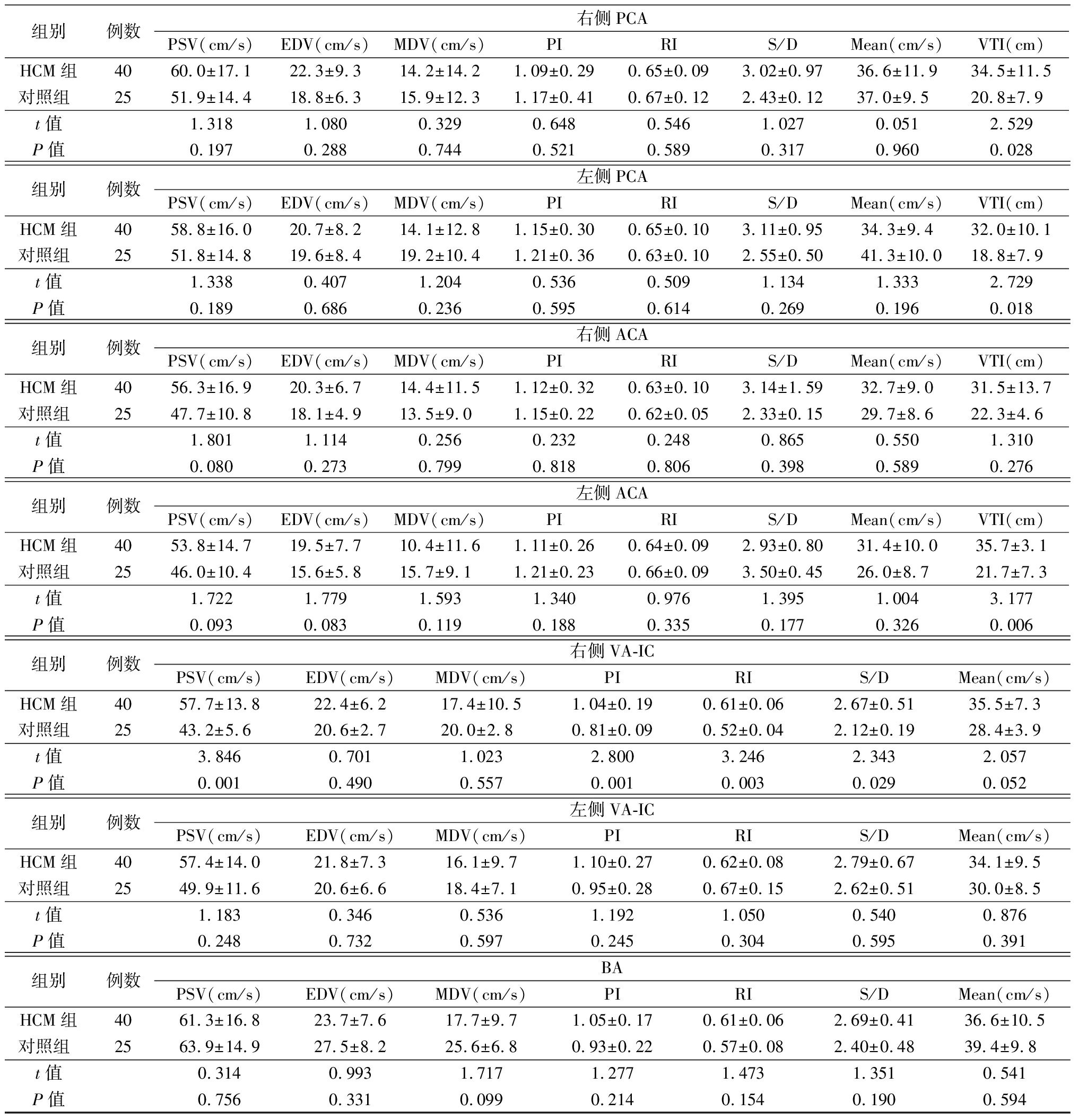
组别例数右侧PCAPSV(cm/s)EDV(cm/s)MDV(cm/s)PIRIS/DMean(cm/s)VTI(cm)HCM组4060.0±17.122.3±9.314.2±14.21.09±0.290.65±0.093.02±0.9736.6±11.934.5±11.5对照组 2551.9±14.418.8±6.315.9±12.31.17±0.410.67±0.122.43±0.1237.0±9.520.8±7.9t值1.3181.0800.3290.6480.5461.0270.0512.529P值0.1970.2880.7440.5210.5890.3170.9600.028组别例数左侧PCAPSV(cm/s)EDV(cm/s)MDV(cm/s)PIRIS/DMean(cm/s)VTI(cm)HCM组4058.8±16.020.7±8.214.1±12.81.15±0.300.65±0.103.11±0.9534.3±9.432.0±10.1对照组 2551.8±14.819.6±8.419.2±10.41.21±0.360.63±0.102.55±0.5041.3±10.018.8±7.9t值1.3380.4071.2040.5360.5091.1341.3332.729P值0.1890.6860.2360.5950.6140.2690.1960.018组别例数右侧ACAPSV(cm/s)EDV(cm/s)MDV(cm/s)PIRIS/DMean(cm/s)VTI(cm)HCM组4056.3±16.920.3±6.714.4±11.51.12±0.320.63±0.103.14±1.5932.7±9.031.5±13.7对照组 2547.7±10.818.1±4.913.5±9.01.15±0.220.62±0.052.33±0.1529.7±8.622.3±4.6t值1.8011.1140.2560.2320.2480.8650.5501.310P值0.0800.2730.7990.8180.8060.3980.5890.276组别例数左侧ACAPSV(cm/s)EDV(cm/s)MDV(cm/s)PIRIS/DMean(cm/s)VTI(cm)HCM组4053.8±14.719.5±7.710.4±11.61.11±0.260.64±0.092.93±0.8031.4±10.035.7±3.1对照组 2546.0±10.415.6±5.815.7±9.11.21±0.230.66±0.093.50±0.4526.0±8.721.7±7.3t值1.7221.7791.5931.3400.9761.3951.0043.177P值0.0930.0830.1190.1880.3350.1770.3260.006组别例数右侧VA-ICPSV(cm/s)EDV(cm/s)MDV(cm/s)PIRIS/DMean(cm/s)HCM组4057.7±13.822.4±6.217.4±10.51.04±0.190.61±0.062.67±0.5135.5±7.3对照组 2543.2±5.620.6±2.720.0±2.80.81±0.090.52±0.042.12±0.1928.4±3.9t值3.8460.7011.0232.8003.2462.3432.057P值0.0010.4900.5570.0010.0030.0290.052组别例数左侧VA-ICPSV(cm/s)EDV(cm/s)MDV(cm/s)PIRIS/DMean(cm/s)HCM组4057.4±14.021.8±7.316.1±9.71.10±0.270.62±0.082.79±0.6734.1±9.5对照组 2549.9±11.620.6±6.618.4±7.10.95±0.280.67±0.152.62±0.5130.0±8.5t值1.1830.3460.5361.1921.0500.5400.876P值0.2480.7320.5970.2450.3040.5950.391组别例数BAPSV(cm/s)EDV(cm/s)MDV(cm/s)PIRIS/DMean(cm/s)HCM组4061.3±16.823.7±7.617.7±9.71.05±0.170.61±0.062.69±0.4136.6±10.5对照组 2563.9±14.927.5±8.225.6±6.80.93±0.220.57±0.082.40±0.4839.4±9.8t值0.3140.9931.7171.2771.4731.3510.541P值0.7560.3310.0990.2140.1540.1900.594
3 讨 论
HCM作为最常见的遗传性心血管疾病,临床表现多样,除常见的心悸、胸闷、胸痛、心律失常等症状,还存在诸多心脏以外的表现,如头晕、黑矇、晕厥、运动过程中血压异常等。因此,对HCM的全面评估还应考虑外周血管,特别是脑供血动脉(颈动脉和椎动脉)和颅脑动脉的血流特征,以及外周血管对心脏的影响。近年来,颈脑血流动力学特征在冠心病[7-8]、扩张性心肌病[9]、心力衰竭[10-12]等均进行相关研究,但在HCM患者中鲜有报道。故本研究采用彩色多普勒超声技术对HCM患者和正常人的心脏、颈部和颅脑血管超声参数进行测量并比较,重点探讨HCM患者颈脑血流动力学变化。
本研究结果显示,HCM组双侧CCA和右侧ICA的EDV、MDV和VTI均低于对照组,表明舒张末期流速降低、血流量减少;PI和RI均高于对照组,表明血管的弹性和顺应性降低。考虑为HCM患者左心室壁增厚、左心室顺应性降低、左心室流出道梗阻所致高阻力血流动力学改变,造成心排血量降低、体循环血量减低、颈部血管血流量不足。文献报道,HCM患者颈动脉搏动的典型双峰脉,也称为重搏,向上的颈动脉搏动波和紧跟其后的第二个峰,
系左心室过度收缩所致[8]。而HCM双侧BA的血流量在无明显降低的情况下,PI和RI高于对照组,提示远心端血管的弹性和顺应性降低。关于颅脑动脉,本研究发现大多数血流动力学参数在HCM和对照组差异均无统计学意义。脑血流灌注的调节受较多因素影响[13-14],可以通过机体神经调节、血流代谢耦联调节及自身调节等多种模式,即在心排血量和颈部血管供血量减低的情况下,仍保持脑血流灌注相对稳定[15-16]。此外,受颅内血管特殊解剖关系的影响,颅内大脑动脉环对前后循环的脑血流具有代偿功能,故导致HCM患者颅脑动脉血流参数与正常对照组差异无统计学意义。
本研究的局限性为纳入病例数较少,颈脑血流量是通过评估相应动脉血流速度、血流速度时间积分以及动脉弹性等间接获得的,故本研究是对HCM患者颈脑血流动力学变化的初步探讨,现有结果需在未来多中心和大样本研究中进一步验证。
综上所述,HCM除心脏功能改变之外,患者颈部血管血流动力学参数也会出现异常。因此,HCM患者应常规进行颈部血管超声筛查,这对全面临床评估和早期干预具有重要意义。
[1] Semsarian C,Ingles J,Maron MS,et al. New perspectives on the prevalence of hypertrophic cardiomyopathy[J]. J Am Coll Cardiol,2015,65(12):1249-1254.
[2] 陈治松,熊丹群,徐文俊,等.肥厚型心肌病患者发生晕厥的危险因素分析[J].中国心脏起搏与心电生理杂志,2016,30(3):234-237.
[3] 沈亦时,傅国胜,孙雅逊.肥厚型心肌病的诊疗进展[J].临床心电学杂志,2018,27(1):49-54.
[4] Authors/Task Force members,Elliott PM,Anastasakis A,et al. 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy:the task force for the diagnosis and management of hypertrophic cardiomyopathy of the European Society of Cardiology(ESC)[J]. Eur Heart J,2014,35(39):2733-2779.
[5] Lang RM,Badano LP,Mor-Avi V,et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging[J]. Eur Heart J Cardiovasc Imaging,2015,16(3):233-270.
[6] 中国医师协会超声医师分会.血管与浅表器官超声检查指南[M].北京:人民军医出版社,2015:9.
[7] 杨旭丽,高虹,罗韶金,等.心源性晕厥的诊断和评估[J].现代医院,2015,15(1):71-74.
[8] Ozdemir O,Soylu M,Durmaz T,et al. Early haemodynamic changes in cerebral blood flow after cardiac resychronisation therapy[J]. Heart Lung Circ,2013,22(4):260-264.
[9] 陈鹏飞,袁丽君,赵联璧,等.扩张型心肌病患者脑血流动力学及认知功能变化超声研究[J].中国超声医学杂志,2017,33(4):289-292.
[10] Kim MS,Kim JS,Yun SC,et al. Association of cerebral blood flow with the development of cardiac death or urgent heart transplantion in patients with systolic heart failure[J]. Eur Heart J,2012,33(3):354-362.
[11] Erkelens CD,van der Wal HH,de Jong BM,et al. Dynamics of cerebral blood flow in patients with mild non-ischaemic heart failure[J]. Eur J Heart Fail,2017,19(2):261-268.
[12] Camaioni C,Knott KD,Augusto JB,et al. Inline perfusion mapping provides insights into the disease mechanism in hypertrophic cardiomyopathy[J]. Heart,2019[Epub ahead of print].
[13] Mitchell C,Korcarz CE,Gepner AD,et al. Ultrasound carotid plaque features,cardiovascular disease risk factors and events:the multi-ethnic study of atherosclerosis[J]. Atherosclerosis,2018,27(6):195-202.
[14] Duffin J,Sobczyk O,McKetton L,et al. Cerebrovascular resistance: the basis of cerebrovascular reactivity[J]. Front Neurosci,2018,12:409.
[15] Aaslid R,Markwalder TM,Nornes H,et al. Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries[J]. J Neurosurg,1982,57(7):769-774.
[16] Willie CK,Tzeng YC,Fisher JA,et al. Integrative regulation of human brain blood flow[J]. J Physiol,2014,592(5):841-859.