子宫腺肌瘤是常见病和多发病,临床上主要表现为痛经、月经增多和不孕等症状,治疗一直选择子宫切除术的方法,但随着对生育能力和保存器官完整性愿望的增加,更多女性患者要求保留子宫[1]。近年来发现子宫动脉栓塞术能够明显改善子宫腺肌瘤的症状,但仍有20%患者无效,故常采用腹腔镜下子宫动脉阻断术[2]。有研究显示左炔诺孕酮宫内节育系统(曼月乐)能够明显降低子宫腺肌瘤的症状和复发率[3]。本研究采用腹腔镜下子宫动脉阻断加子宫腺肌瘤切除术联合曼月乐治疗子宫腺肌瘤取得较好的效果,报告如下。
1 资料与方法
1.1 一般资料 选择2013年1月—2016年12月在我院就诊的子宫腺肌瘤患者130例,均符合子宫腺肌瘤的诊断,随机分为观察组和对照组各65例。观察组年龄28~45岁,平均(36.58±2.37)岁,病程2~6年,平均(3.64±1.35)年,平均孕次(2.35±0.68)次,平均产次(1.23±0.24)次。对照组26~47岁,平均(36.78±2.19)岁,病程2~6年,平均(3.59±1.27)年,平均孕次(2.29±0.58)次,平均产次(1.19±0.29)次。纳入标准:子宫增加>8周;均有手术指征;患者均知情同意;本研究经医院医学伦理委员会通过。排除标准:合并有卵巢子宫内膜异位;恶性肿瘤;血液系统疾病和免疫性疾病;心肝肾等重要脏器不全患者;肝炎、结核和肺炎等急慢性感染性疾病。2组年龄、病程、产次和孕次等差异均无统计学意义(P>0.05),具有可比性。
1.2 方法
1.2.1 治疗方法 2组均给予腹腔镜子宫动脉阻断加子宫腺肌瘤切除,对照组给予米非司酮治疗,观察组给予曼月乐治疗。具体用法:米非司酮 12 mg 口服,每天1次,疗程3个月;治疗后第1次月经来潮的第3~7天,宫内放置曼月乐(左炔诺孕酮,52 mg)治疗。腹腔镜子宫动脉阻断加子宫腺肌瘤切除:患者均在全身麻醉下,采用3孔法,置入腹腔镜器械后,经阴道置入举宫器,分离子宫周围粘连,阻断子宫动脉;双侧子宫动脉阻断后子宫呈暗紫色,行子宫腺肌瘤病灶切除,对于弥漫性病灶切除增厚的肌壁将腺肌瘤病灶一并切除,使子宫体积恢复正常,肉眼无明显病灶,刨面组织弹性恢复。
1.2.2 疗效评价 治疗后12个月评价疗效:主要症状和体征消失为显效;主要症状和体征缓解为有效;主要症状和体征无明显变化为无效。总有效率=(有效+显效)例数/总例数×100%。
1.2.3 子宫体积和痛经程度评分 术前和治疗后12个月,在月经后3~7 d用超声测量子宫体积,子宫体积=0.523×子宫三个维径的半径乘积(cm3)。痛经程度评分:根据患者疼痛程度分为0~10分,无痛觉为0分,分数越高表明疼痛越明显、越严重[4]。
1.2.4 激素水平检测 术前和治疗后12个月,取患者肘正中静脉血约10 mL,以2 500 r/min离心(离心半径6 cm)约10 min,分离出上清液放置于-80 ℃冰箱中保存。应用电化学发光仪(瑞士罗氏公司)检测糖抗原125(carbohydrate antigen 125,CA125)、黄体生成激素(luteinizing hormone,LH)、促卵泡成熟激素(follicle-stimulating hormone,FSH)和雌二醇(estradiol,E2),采用Elecsys软件自动通过定标曲线计算出CA125、LH、FSH和E2含量。
1.2.5 观察指标 观察2组疗效和不良反应发生率;比较2组治疗前和治疗后12个月子宫体积、宫腔大小、CA125、月经情况,以及LH、FSH和E2的变化。
1.3 统计学方法 应用SPSS 12.0统计软件分析数据。计量资料比较分别采用两独立样本的t检验和配对t检验;计数资料比较采用χ2检验;等级资料比较采用秩和检验。P<0.05为差异有统计学意义。
2 结 果
2.1 2组临床疗效和总有效率比较 观察组临床疗效和总有效率均高于对照组,差异有统计学意义(P<0.05),见表1。
表1 2组疗效和总有效率比较
Table 1 Comparison of curative effect and total effective rate between two groups (n=65,例数,%)
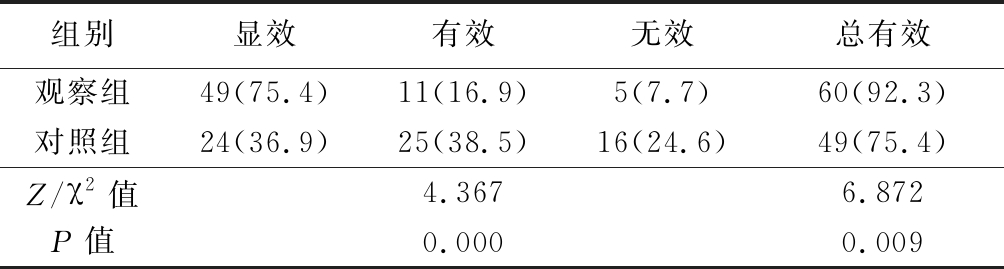
组别显效有效无效总有效观察组49(75.4)11(16.9) 5(7.7)60(92.3)对照组24(36.9)25(38.5)16(24.6)49(75.4)Z/χ2值4.3676.872P值0.0000.009
2.2 2组子宫体积、宫腔大小和CA125水平比较 治疗前2组子宫体积、宫腔大小和CA125水平差异均无统计学意义(P>0.05);治疗后2组子宫体积、宫腔大小和CA125水平均较治疗前明显缩小或降低(P<0.05),观察组缩小和降低的幅度更大,治疗后观察组子宫体积、宫腔大小和CA125水平均小于或低于对照组(P<0.05)。见表2。
表2 2组子宫体积、宫腔大小和CA125水平比较
Table 2 Comparison of uterus volume, uterine cavity size and CA125 between two groups![]()
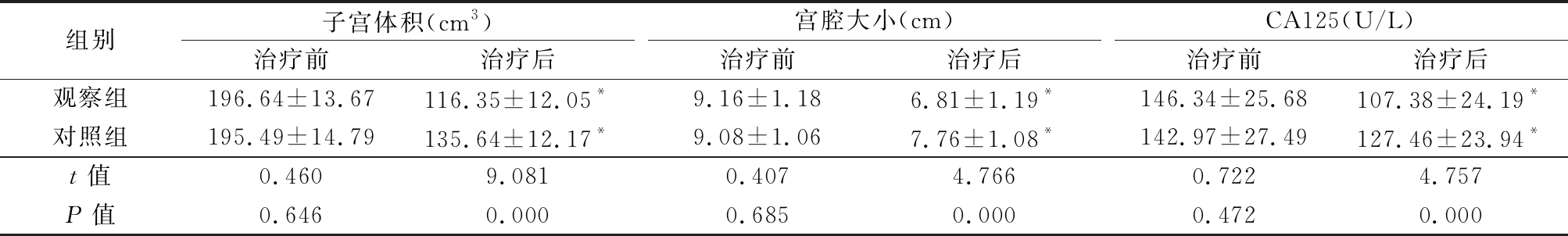
组别子宫体积(cm3)治疗前治疗后宫腔大小(cm)治疗前治疗后CA125(U/L)治疗前治疗后观察组196.64±13.67116.35±12.05*9.16±1.186.81±1.19*146.34±25.68107.38±24.19*对照组195.49±14.79135.64±12.17*9.08±1.067.76±1.08*142.97±27.49127.46±23.94*t值0.4609.0810.4074.7660.7224.757P值0.6460.0000.6850.0000.4720.000
*P值<0.05与治疗前比较(配对t检验)
2.3 2组治疗前后月经情况变化 治疗前2组月经期、月经周期和疼痛评分差异均无统计学意义(P>0.05);治疗后2组月经期均明显缩短,疼痛评分均较治疗前明显降低,月经周期均较治疗前明显延长(P<0.05),治疗后观察组疼痛评分低于对照组(P<0.05),治疗后2组月经期和月经周期差异均无统计学意义(P>0.05)。见表3。
表3 2组治疗前后月经情况变化
Table 3 Changes of menstrual conditions before and after treatment between two groups![]()
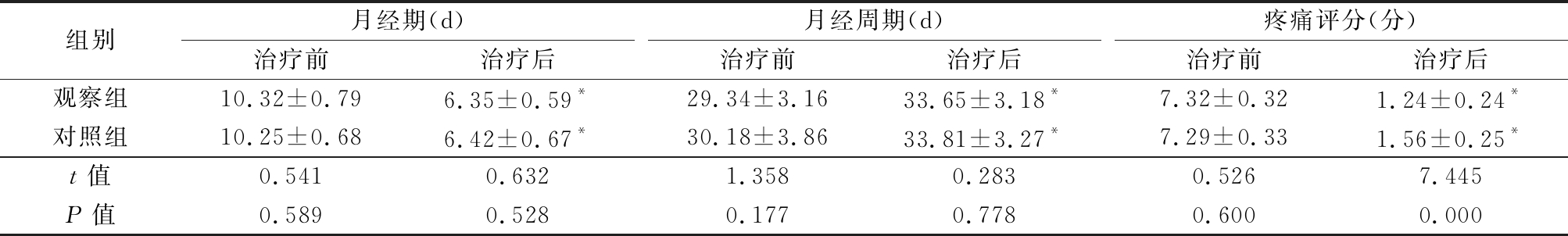
组别月经期(d)治疗前治疗后月经周期(d)治疗前治疗后疼痛评分(分)治疗前治疗后观察组10.32±0.796.35±0.59*29.34±3.1633.65±3.18*7.32±0.321.24±0.24*对照组10.25±0.686.42±0.67*30.18±3.8633.81±3.27*7.29±0.331.56±0.25*t值0.5410.6321.3580.2830.5267.445P值0.5890.5280.1770.7780.6000.000
*P值<0.05与治疗前比较(配对t检验)
2.4 2组治疗前后卵巢功能变化 治疗前2组LH、FSH和E2水平差异均无统计学意义(P>0.05);治疗后2组LH、FSH水平均较治疗前明显降低,E2水平均较治疗前明显升高(P<0.05),治疗后观察组LH、FSH和E2水平均低于对照组(P<0.05)。见表4。
表4 2组治疗前后卵巢功能变化比较
Table 4 Comparison of ovarian function before and after treatment between two groups![]()
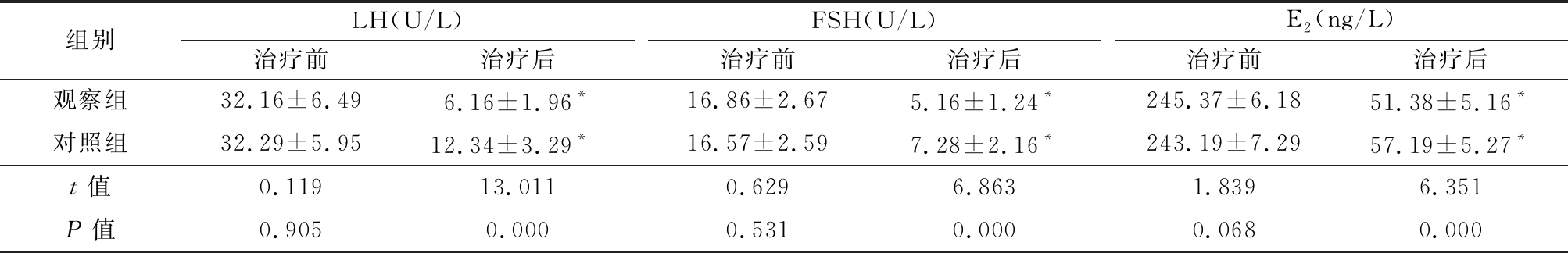
组别LH(U/L)治疗前治疗后FSH(U/L)治疗前治疗后E2(ng/L)治疗前治疗后观察组32.16±6.496.16±1.96*16.86±2.675.16±1.24*245.37±6.1851.38±5.16*对照组32.29±5.9512.34±3.29*16.57±2.597.28±2.16*243.19±7.2957.19±5.27*t值0.11913.0110.6296.8631.8396.351P值0.9050.0000.5310.0000.0680.000
*P值<0.05与治疗前比较(配对t检验)
2.5 2组不良反应比较 观察组在治疗过程中出现闭经1例、乳房胀痛1例、不规则出血2例、月经稀少2例,不良反应发生率为9.23%(6/65);对照组治疗过程中出现闭经2例、乳房胀痛3例、不规则出血1例、月经稀少2例,不良反应发生率为12.31%(8/65)。2组不良反应发生率差异无统计学意义(χ2=0.342,P>0.05)。
3 讨 论
子宫腺肌瘤最终的治疗手段是子宫切除,疗效肯定,但现代医学认为子宫作为人体的重要器官,保留子宫具有重要的临床意义[4-5]:子宫可以产生多种活性物质,是重要的内分泌器官;避免了切除子宫过程中对卵巢的血液供应,同时可以减少粘连引起的残留卵巢综合征;减少患者盆底松弛,保留子宫和卵巢功能。近年的研究表明手术中行子宫动脉阻断术能够减少子宫动脉的血液供应,使异位病灶缺血缺氧,从而达到缓解痛经和减少月经量的目的[6-7]。有研究证实腹腔镜下子宫腺肌瘤切除术联合子宫动脉阻断术治疗子宫腺肌瘤效果显著,但其仍有一定的复发率[6]。曼月乐为左炔诺孕酮宫内缓释系统,是一种缓释系统,每天释放左炔诺孕酮20 μg在宫腔内,可以持续使用5年,以往主要用于避孕,以及月经过多、痛经和绝经后激素替代疗法,其主要作用机制是释放到宫腔内的左炔诺孕酮直接作用子宫内膜,抑制雌激素受体的合成,使子宫内膜失去E2的敏感性,导致内膜变薄,月经量减少,抑制异位内膜生长和活性,可以明显减轻痛经程度。左炔诺孕酮能够减少子宫内膜产生前列腺素和血栓素,消除子宫平滑肌痉挛收缩,从而减少子宫体积[1,8]。本研究结果显示腹腔镜下子宫腺肌瘤切除联合子宫动脉阻断加曼月乐治疗子宫腺肌瘤的效果明显优于非用曼月乐治疗的患者,观察组缩小子宫体积和宫腔大小较对照组更加明显,且在改善患者痛经方面也更优。
本研究观察组CA125水平明显低于对照组。CA125是一种体腔内上皮大相对分子质量的多聚糖蛋白,并且不随月经的变化而变化,其随子宫腺肌瘤严重程度增加而升高,异位症患者水平是正常组织含量的2~4倍[9-11]。本研究表明曼月乐联合手术能够控制血液CA125水平。子宫腺肌瘤使用米非司酮后疗效确切,但患者的依赖性较强,一旦停药即会复发。卵巢储备功能的敏感指标为E2和FSH,二者结合预测卵巢储备功能更为可靠。卵巢血流与储备功能关系密切,子宫动脉结扎术能够使侵入子宫肌层的子宫内膜异位灶出现坏死、溶解和吸收,从而达到治疗子宫内膜异位灶的目的[12-13]。同时在腹腔镜子宫动脉结扎直视下操作,对卵巢动脉误伤的可能性极少,对卵巢的血供没有影响,对卵巢功能无明显影响。曼月乐是节育器的一种,刚开始用于避孕,后来运用于治疗子宫腺肌瘤并有较好的疗效,在临床得到广泛运用。本研究结果显示手术联合曼月乐能够明显降低机体血清FSH、LH和E2水平。其可能的机制是曼月乐使在位内膜孕激素的浓度为异位内膜的100倍,并通过孕激素的负反馈,减少病灶中的E2受体,减弱了E2的作用,同时具有明显抑制卵巢和睾丸对促性腺激素的反应,降低机体E2和睾酮的生成,促进异位内膜萎缩,对异位内膜的种植和侵袭具有重要抑制作用,增加子宫动脉阻力,减少子宫血流量,减少经血碎片中活细胞的数量,减少内膜中前列腺素的产生,对痛经具有明显的缓解作用[14-15]。本研究表明曼月乐联合手术治疗能够明显降低机体血清性激素水平,对患者的卵巢功能具有明显改善作用。
总之,腹腔镜子宫动脉阻断加子宫腺肌瘤切除合并曼月乐治疗子宫腺肌瘤效果显著,能够明显缓解症状和改善卵巢功能。
[1] Lin CJ,Hsu TF,Chang YH,et al. Postoperative maintenance levonorgestrel-releasing intrauterine system for symptomatic uterine adenomyoma[J]. Taiwan J Obstet Gynecol,2018,57(1):47-51.
[2] Chen L,Li C,Guo J,et al. Eutopic/ectopic endometrial apoptosis initiated by bilateral uterine artery occlusion:a new therapeutic mechanism for uterus-sparing surgery in adenomyosis[J]. PLoS One,2017,12(4):e0175511.
[3] de Bruijn AM,Smink M,Lohle PNM,et al. Uterine artery embolization for the treatment of adenomyosis: a systematic review and meta-analysis[J]. J Vasc Interv Radiol,2017,28(12):1629-1642.
[4] Lindheim SR. Chronic pelvic pain: presumptive diagnosis and therapy using GnRHagonists[J]. Int J Fertil Womens Med,1999,44(3):131-138.
[5] 胡程.子宫全切术与子宫肌瘤剔除术治疗子宫肌瘤的效果及其对卵巢功能影响的对比探讨[J].河北医科大学学报,2016,37(9):1090-1092.
[6] Yang W,Liu M,Liu L,et al. Uterine-sparing laparoscopic pelvic plexus ablation,uterine artery occlusion,and partial adenomyomectomy for adenomyosis[J]. J Minim Invasive Gynecol,2017,24(6):940-945.
[7] 蓝洁珍,刘娇兰.双侧子宫动脉上行支结扎+改良式子宫背带式缝合术在剖宫产术难治性产后出血中的应用[J].河北医科大学学报,2018,39(3):301-304.
[8] Vannuccini S,Luisi S,Tosti C,et al. Role of medical therapy in the management of uterine adenomyosis[J]. Fertil Steril,2018,109(3):398-405.
[9] Calagna G,Cucinella G,Tonni G,et al. Cystic adenomyosis spreading into subserosal-peduncolated myoma: How to explain it?[J]. Int J Surg Case Rep,2015,8C:29-31.
[10] Kil K,Chung J,Pak HJ,et al. Usefulness of CA125 in the differential diagnosis of uterine adenomyosis and myoma[J]. Eur J Obstet Gynecol Reprod Biol,2015,185:131-135.
[11] Xiao Y,Li T,Xia E,et al. Expression of integrin β3 and osteopontin in the eutopic endometrium of adenomyosis during the implantation window[J]. Eur J Obstet Gynecol Reprod Biol,2013,170(2):419-422.
[12] 赵剑虹,蒋希菁,沈岚,等.腹腔镜下子宫动脉阻断联合腺肌瘤剥除术治疗子宫腺肌瘤的可行性探讨[J].中国内镜杂志,2014,20(4):372-375.
[13] 成九梅,段华,刘芸,等.腹腔镜下子宫腺肌病灶挖除及子宫动脉阻断治疗子宫腺肌病的长期疗效分析[J].北京医学,2014,36(1):19-23.
[14] Struble J,Reid S,Bedaiwy MA. Adenomyosis:a clinical review of a challenging gynecologic condition[J]. J Minim Invasive Gynecol,2016,23(2):164-185.
[15] Benagiano G,Brosens I,Habiba M. Structural and molecular features of the endomyometrium in endometriosis and adenomyosis[J]. Hum Reprod Update,2014,20(3):386-402.