脊髓型颈椎病常因颈椎椎体、椎间盘、椎间关节及相关的韧带退变引起骨赘形成,椎间隙塌陷,严重者可出现脊髓压迫和受损,其发病年龄为40~60岁[1]。脊髓型颈椎病发病隐匿,患者就诊时已出现不同程度的脊髓压迫症状,如皮肤感觉减退、双下肢无力、行走不稳、双上肢精细功能降低等。随着患者病程延长,常规MRI检查出现髓内T2高信号,查体Hoffman征和Babinski征阳性时,虽然经过手术使脊髓彻底减压,但是预后较差,往往残留部分神经功能损伤症状。临床研究证实,脊髓T2WI信号比值(signal intensity ratio,SIR)能够反映脊髓功能变化,并且对患者转归有一定指导意义[2-3]。同时,脊髓长期受压后,脊髓白质少突胶质细胞及脊髓灰质神经元细胞均有不同程度的凋亡,脊髓受压时间越长,细胞凋亡越严重,SIR与脊髓细胞凋亡程度显著相关[4]。另一项 MRI 检查,扩散张量成像(diffusion tensor imaging,DTI)可以有效观察脊髓病变及再生修复的动态过程,进行组织的微观结构改变定量分析,并且纤维束示踪成像技术可以立体展现白质纤维束形态,可以为临床工作提供许多更有价值的信息[5]。本研究选择不同程度SIR脊髓型颈椎病患者37例,通过观察其脊髓功能及FA值变化,探索FA值对SIR显著升高的脊髓型颈椎病的诊断价值。
1 资料与方法
1.1 一般资料 选择2014年1月—2015年1月我院收治的脊髓型颈椎病患者37例。纳入标准:①行颈椎1.5T MRI检查,显示脊髓受压;②测量受压最显著部位T2WI信号强度与C7/T1节段脊髓内信号强度的比值,SIR升高。患者均由1名脊柱外科医师查体,并记录日本矫形外科协会(Japanese Orthopaedic Association,JOA)评分及专科查体结果。排除标准:①先天性椎管狭窄;②颈椎后纵韧带骨化;③颈椎外伤;④多节段椎间盘突出(>3个节段);⑤伴有明显颈椎不稳;⑥脊髓变性疾病,如多发性硬化;⑦有四肢关节疾病,影响上下肢运动功能;⑧C7/T1水平脊髓信号改变。
根据术前脊髓T2WI信号比值(signal intensity ratio,SIR)分为3组:A 组11例, SIR<1.32;B 组12例,SIR 1.32~1.68;C 组14例, SIR>1.68。A组男性5例,女性6例,年龄41~63岁,平均(54.27±6.26)岁,体重指数(body mass index,BMI)23.91±2.98,病理征阳性9例;B组男性7例,女性5例,年龄39~64岁,平均(55.83±5.57)岁,BMI 24.82±2.74,病理征阳性10例;C组男性9例,女性5例,年龄44~67岁,平均(58.93±6.25)岁,BMI 23.59±2.92,病理征阳性13例。3组性别、年龄、BMI、病理征阳性例数差异均无统计学意义(P>0.05),具有可比性。
1.2 影像学测量 常规MRI检查包括矢状位T1WI、T2WI和横轴位T2WI。矢状位FSE-T1WI序列,参数:TR/TE 550/9 ms,层厚3 mm,层间距0.3 mm,视野240 mm×240 mm,矩阵320×240,AverageS;矢状位FRFSE-T2WI序列,参数:TR/TE 3 800/108 ms,层厚3 mm,层间距0.3 mm,FOV 240 mm×240 mm,矩阵384×286,Aerage2;横轴位T2WI 序列,参数:TR/TE 3 000/90 ms,层厚3 mm,层间距 0.3 mm,FOV 180 mm×180 mm,矩阵 320×240,带宽284 kHz,Average10。
SIR测量:选取受压节段最重的节段,以该处矢状位脊髓的0.05 cm2作为测量范围,测量T2WI的数值(a),记录C7/T1作为正常节段测量并以该段脊髓的0.3 cm2作为测量范围,记录该处的T2WI信号值(b),SIR=a/b。
DTI 检测方法:患者均采用快速扰相位梯度回波序列进行定位扫描,使用快速自旋回波序列完成矢状面T2WI及T1WI扫描。扫描参数 T2WI:TR/TE 3 280 ms/98 ms,T1WI:TR/TE 501/11 ms,层厚3.0 mm,FOV 280 mm×250 mm,采集矩阵120×128。采用SIEMENS公司的3.0T MAG-NETOM Verio,梯度场40 mT/m,切换率200 mT·m-1·ms-1,发射线圈使用体线圈,接受线圈采用四通道相控阵脊柱线圈,测量部分各向异性(fractional anisotropy,FA)值。
1.3 脊髓功能评估 应用JOA评分评估患者脊髓功能,JOA 评分改善率=(术后 JOA 评分-术前 JOA 评分)/(17-术前 JOA 评分)×100%。在此基础上,细化上下肢功能的临床检测方法[6]:①正常步长6 m行走时间,在室内测量出6 m长距离,分别标出起点线及终点线,测量患者由起点线开始自然步态行走到终点线所用的时间;②最大步长6 m行走时间,测量6 m距离,患者由起点开始以最大步长行走至终点线,测量患者行走6 m所需的时间;③5次连续坐起时间,取一把常用的无扶手椅子,请受试者连续进行5次坐下站起动作,记录受试者连续完成 5 次坐下站起动作所需的时间。以60 s作为时间的上限,如果受试者在60 s内未能完成5次坐下站起动作,该受试者的时间记录为60 s;④10 s连续握松拳次数,记录10 s内患者左右手握拳并松开动作往复运动总共完成的次数,最终结果记录左右手完成次数的均值。
1.4 脊髓病理征评估 膝腱反射亢进,Hoffman征(+), Babinski征(+),其中至少1个体征出现即认为病理征阳性
1.5 治疗及随访 颈椎病患者均接受颈前路减压植骨融合内固定手术,采用自体骨植骨融合。术后患者颈托固定,早期开始功能锻炼,术后24 h下地活动,48 h取出引流条,术后8~9 d拆除缝线,术后2个月摘除颈托。所有患者于术后3个月、6个月、1年和2年随访,至少随访2年。随访时,记录患者JOA评分、正常步长6 m行走时间、最大步长6 m行走时间、5次连续坐下站起所用时间和连续紧握-松开双手次数。观察脊髓功能恢复情况。并于术后1年时复查颈椎MRI,因患者接受手术治疗术后局部结构破坏并有内固定物植入,DTI检查受干扰,精确性降低,故术后仅行MRI检查而未行DTI检查。
1.6 统计学方法 应用 SPSS 22.0统计软件分析数据。计量资料比较采用配对t检验、F检验和SNK-q检验;计数资料比较采用χ2检验;相关性采用Pearson检验。P<0.05为差异有统计学意义。
2 结 果
2.1 3组临床情况比较 3组均顺利完成手术。3组间手术时间、出血量、脑脊液漏发生率差异均无统计学意义(P>0.05);C组FA值低于A组和B组(P<0.05)。见表1。
表1 3组临床情况比较
Table 1 Comparison of clinical conditions among 3 groups![]()
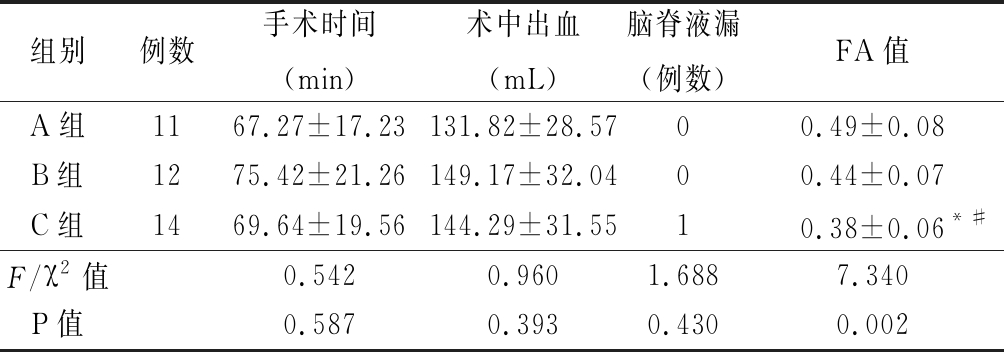
组别例数手术时间(min)术中出血(mL)脑脊液漏(例数)FA值A组1167.27±17.23131.82±28.5700.49±0.08B组1275.42±21.26149.17±32.0400.44±0.07C组1469.64±19.56144.29±31.5510.38±0.06*#F/χ2值0.5420.9601.6887.340P值0.5870.3930.4300.002
*P值<0.05与A组比较 #P值<0.05与B组比较(SNK-q检验)
2.2 3组脊髓功能比较 术前和随访时,C组JOA评分低于A组和B组,3组随访时JOA评分高于术前,C组JOA评分改善率低于A组(P<0.05)。术前和随访时,C组正常步长 6 m行走时间长于A组和B组,3组随访时正常步长 6 m行走时间短于术前(P<0.05)。术前,B组最大步长6 m行走时间长于A组,C组最大步长6 m行走时间长于A组和B组,随访时,C组最大步长6 m行走时间长于A组,3组随访时最大步长6 m行走时间短于术前(P<0.05)。术前,C组5次连续坐起时间长于A组和B组,随访时,B组5次连续坐起时间长于A组,C组5次连续坐起时间长于A组和B组,3组随访时5次连续坐起时间短于术前(P<0.05)。术前和随访时,C组10 s连续握松拳次数少于A组,3组随访时10 s连续握松拳次数多于术前(P<0.05)。见表2。
表2 3组脊髓功能比较
Table 2 Comparison of spinal function among 3 groups![]()

组别例数JOA评分(分)术前随访JOA评分改善率(%)正常步长6 m行走时间(s)术前随访A组1110.55±2.0214.09±2.21*58.37±28.199.18±2.046.73±1.74*B组128.83±2.2112.92±2.68*50.66±30.21 11.33±2.849.17±2.08*C组147.14±1.99#△10.14±2.91*#△30.57±24.39#15.21±3.07#△10.93±3.43*#△F值8.3337.4953.47815.9048.014P值0.0010.0020.0420.0000.001组别例数最大步长6 m行走时间(s)术前随访5次连续坐起时间(s)术前随访10 s连续握松拳次数(次) 术前随访A组117.82±1.606.27±1.42*18.55±2.8815.18±3.19*19.73±2.6922.45±2.98*B组1210.08±2.61#8.08±1.83*21.42±3.7818.58±3.65*#17.33±3.5820.41±3.42*C组1414.07±3.15#△9.79±2.89*#27.14±4.42#△22.57±3.67*#△15.43±3.34#18.14±4.45*#F值18.7637.83116.74413.6645.4014.137P值0.0000.0020.0000.0000.0090.025
*P值<0.05与术前比较(配对t检验) #P值<0.05与A组比较 △P值<0.05与B组比较(SNK-q检验)
2.3 JOA评分与FA值的相关性 术前JOA评分与FA值呈显著正相关(r=0.633,P=0.000);术后JOA评分改善率与FA值之间亦呈显著正相关(r=0.499,P=0.002)。
3 讨 论
脊髓型颈椎病的预后观察主要通过JOA评分评价,但JOA评分有其局限性,为了更精确地反映术前术后脊髓功能的恢复情况,本研究细化了4项针对上下肢运动功能的专科查体检测指标,使查体指标量化,更易于比较各组患者四肢运动功能变化情况。在早期脊髓型颈椎病发病率的流行病学研究中,应用此4项查体结合颈椎MRI检查成功发现社区居民中无明显主观不适症状的早期脊髓型颈椎病患者。本研究结果显示,3组正常步长6 m行走时间、最大步长6 m行走时间、5次连续坐起时间、10 s连续握松拳次数差异均有统计学意义,随访时3组正常步长6 m行走时间、最大步长6 m行走时间、5次连续坐起时间、10 s连续握松拳次数均明显改善。因此,以上4项专科查体能够作为评价脊髓型颈椎病手术疗效的有效指标。目前颈椎MRI检查已成为脊髓型颈椎病诊断的重要检查项目之一,MRI检查不仅能够明确脊髓受压程度,还能够通过MRI信号强度变化判定脊髓受损程度,同时脊髓内T2相高信号也是手术适应证之一和判断预后的重要指标[7]。但也有学者持不同观点,认为单纯的T2高信号并不能提示脊髓功能受损严重,也无法预测患者手术预后,且常规颈椎MRI检查对于早期脊髓损伤的敏感度仅有55%,对于不伴有颈椎MRI的T2WI高信号型颈椎病的早期诊断较困难[5]。随着颈椎病病程的延长和脊髓受压时间增加,脊髓缺血变性,最终导致不可逆的神经损伤。有研究证实,颈椎病病程较长是预后不良的危险因素[2]。故早期诊断、早期治疗对颈椎病的预后有积极作用。DTI检查可以在脊髓损伤患者T2像产生高信号之前显示脊髓损伤程度,为下一步治疗提供指导方案[8]。将常规MRI检查和DTI检查对比研究发现,DTI检查对于早期颈髓损伤诊断更有价值,且受年龄因素干扰较小;在脊髓型颈椎病患者预后预测方面,DTI分级优于MRI分级[9]。应用DTI检查,可以达到早发现、早治疗颈椎病的目的,及时挽救脊髓功能,改善颈椎病预后,提高患者生活质量,对颈椎病的诊断和治疗有重要意义。既往研究发现,随着SIR升高,患者脊髓功能显著降低,轻度中度与重度升高组脊髓功能存在显著性差异。表明SIR强度能够反映脊髓功能受损程度且对术后患者症状改善具有一定预测意义[10]。
本研究在先前研究的基础上,根据SIR升高情况,将患者分为SIR低、中、高组,并于手术前后对3组颈椎应用JOA评分和量化的专科查体(正常步长6 m行走时间、最大步长6 m行走时间、5次连续坐起时间和10 s连续握松拳次数)评价脊髓功能,结果显示SIR越高,脊髓功能越差,术后随访发现术前SIR越高,脊髓预后越差。因此,认为脊髓SIR高低能够提示脊髓功能受损且可预测患者术后脊髓功能恢复情况。
DTI检查长期用于脑组织白质病变的研究,近期逐渐开始应用于脊髓相关疾病的研究。DTI检查能够反映微环境下水分子的弥散度[11-12],扩散张量矩阵,其中的特征向量和特征值,分别显示水分子运动的方向和强度。DTI 检查常用的参数包括表观弥散系数及FA值。受压节段FA值是从弥散张量矩阵导出描述的体素,其各向同性扩散范围从 0%(各向同性扩散)到 100%(单向扩散)。传统MRI检查经常受到各种伪影的干扰,导致图像质量降低,从而影响临床医生对于脊髓型颈椎病患者早期诊断和干预。而DTI检查能够有效避免各种伪影的干扰,提高质量图像,并且提供脊髓显微组织信息,能够定量反映脊髓的病理状态,从而指导临床治疗策略[13]。Vedantam等[14]研究发现,脊髓受压最重节段的FA值显著低于颈1~2正常节段平均值;与术前JOA评分和术后3个月时JOA评分变化幅度呈显著正相关。FA值可以作为诊断脊髓型颈椎病患者的潜在标志物。在多发性硬化的研究中发现FA 值越低,扩散的方向均一性越差,表明轴索脱髓鞘改变的程度越重。在脑部疾病的研究中发现,早期由于细胞外分子进入细胞内造成细胞水肿或细胞外间隙变小,而进一步加重后细胞溶解细胞内分子外流造成血管炎性水肿导致FA值降低[15]。在阿尔茨海默病患者中,神经元纤维缠结、海马锥体细胞颗粒空泡变形和神经元缺失导致FA值降低,通过DTI检查可以指导阿尔茨海默病患者的治疗进展或治疗效果[16]。当脊髓型颈椎病患者脊髓受压时,由于长期缺血,白质首先出现脱髓鞘病变,此时DTI检查FA值降低[17]。有研究发现,常规颈椎MRI检查对脊髓损伤的早期诊断敏感度只有55%,而通过DTI检查得到的FA值对脊髓损伤的早期诊断敏感度可达79%,明显优于常规MRI检查[5]。因此,DTI检查对颈椎病的早期诊断有重要意义。本研究结果显示,FA值与术后JOA评分以及JOA评分改善率均有相关性。说明FA值能一定程度反映颈椎病的手术预后。DTI检查对于脊髓型颈椎病患者的早期诊断和治疗方式的选择更有指导意义。
一项脊髓损伤相关研究发现,FA值能够很好地反映脊髓功能的变化,二者有显著相关性[18]。近年来有关脊髓型颈椎病DTI检查的相关研究较多,发现低FA值与脊髓型颈椎病及其症状密切相关[19]。Rao等[20]将DTI检查应用于脊髓型颈椎病患者的术前术后评估,发现术前FA值与JOA评分呈正相关,与术后预后呈现负相关;且将DTI检查对临床预后指标量化,发现术前FA值<0.55的患者,脊髓型颈椎病患者术后预后明显较术前FA值>0.55时的患者差。有研究发现,在未出现T2高信号的脊髓型颈椎病患者中,脊髓压迫严重的患者FA值显著降低,即当无脊髓T2高信号时,FA值可以作为评价患者脊髓压迫程度的指标[21]。以上研究仅将脊髓MRI T2信号定性地分为有无升高,而本研究将SIR定量分组,能够更加准确反映各组之间脊髓受损程度,通过比较不同程度SIR患者FA值的变化,进一步验证了FA值与脊髓功能改变的一致性和FA值对脊髓功能恢复程度的预测能力。
[1] Wang MC,Chan L,Maiman DJ,et al. Complications and mortality associated with cervical spine surgery for degenerative disease in the united states[J]. Spine(Phila Pa 1976),2007,32(3):342-347.
[2] Zhang J,Cui C,Liu Z,et al. Predisposing factors for poor outcome of surgery for cervical spondylotic amyotrophy:a multivariate analysis[J]. Sci Rep,2016,6:39512.
[3] Wei L,Cao P,Xu C,et al. Comparison of the prognostic value of different quantitative measurements of increased signal intensity on T2-weighted MRI in cervical spondylotic myelopathy[J]. World Neurosurg,2018,118:e505-512.
[4] Ma L,Zhang D,Chen W,et al. Correlation between magnetic resonance T2 image signal intensity ratio and cell apoptosis in a rabbit spinal cord cervical myelopathy model[J]. Chin Med J,2014,127(2):305-313.
[5] Shabani S,Kaushal M,Budde M,et al. Comparison between quantitative measurements of diffusion tensor imaging and T2 signal intensity in a largeseries of cervical spondylotic myelopathy patients for assessment of diseaseseverity and prognostication of recovery [J]. J Neurosurg Spine,2019,7:1-7.
[6] Jung H,Yamasaki M. Association of lower extremity range of motion and muscle strength with physical performance of community-dwelling older women[J]. J Physiol Anthropol,2016,35(1):30.
[7] Machino M,Ando K,Kobayashi K,et al. Alterations in intramedullary T2-weighted increased signal intensity following laminoplasty in cervical spondylotic myelopathy patients:comparison between pre-and postoperative magnetic resonance images[J]. Spine(Phila Pa 1976),2018,43(22):1595-1601.
[8] Liu Y,Kong C,Cui L,et al. Correlation between diffusion tensor imaging parameters and clinical assessments in patients with cervical spondylotic myelopathy with and without high signal intensity[J]. Spinal Cord,2017,55(12):1079-1083.
[9] Wang K,Chen Z,Zhang F,et al. Evaluation of DTI parameter ratios and diffusion tensor tractography grading in the diagnosis and prognosis prediction of cervical spondylotic myelopathy[J]. Spine(Phila Pa 1976),2017,42(4):E202-210.
[10] Zhang YZ,Shen Y,Wang LF,et al. Magnetic resonance T2 image signal intensity ratio and clinical manifestation predict prognosis after surgical intervention for cervical spondylotic myelopathy[J]. Spine(Phila Pa 1976),2010,35(10):E396-399.
[11] Maki S,Koda M,Kitamura M,et al. Diffusion tensor imaging can predict surgical outcomes of patients with cervical compression myelopathy[J]. Eur Spine J,2017,26(9):2459-2466.
[12] Shen C,Xu H,Xu B,et al. Value of conventional MRI and diffusion tensor imaging parameters in predicting surgical outcome in patients with degenerative cervical myelopathy[J]. J Back Musculoskelet Rehabil,2018,31(3):525-532.
[13] Guan L,Chen X,Hai Y,et al. High-resolution diffusion tensor imaging in cervical spondylotic myelopathy:a preliminary follow-up study[J]. NMR Biomed,2017,30(10):e3769.
[14] Vedantam A,Rao A,Kurpad SN,et al. Diffusion tensor imaging correlates with short-term myelopathy outcome in patients with cervical spondylotic myelopathy[J]. World Neurosurg,2017,97:489-494.
[15] Novikov DS,Fieremans E,Jespersen SN,et al. Quantifying brain microstructure with diffusion MRI:theory and parameter estimation[J]. NMR Biomed,2019,32(4):e3998.
[16] Mayo CD,Garcia-Barrera MA,Mazerolle EL,et al. Relationship between DTI metrics and cognitive function in Alzheimer′s disease[J]. Front Aging Neurosci,2019,10:436.
[17] Kaushal M,Shabani S,Budde M,et al. Diffusion tensor imaging in acute spinal cord injury:a review of animal and human studies[J]. J Neurotrauma,2019,36(15):2279-2286.
[18] Poplawski MM,Alizadeh M,Oleson CV,et al. Application of diffusion tensor imaging in forecasting neurological injury and recovery after human cervical spinal cord injury[J]. J Neurotrauma,2019,36(21):3051-3061.
[19] 丁俊,陈基明.扩散张量成像在轻度脊髓型颈椎病诊断中的价值[J].皖南医学院学报,2017,36(3):270-273.
[20] Rao A,Soliman H,Kaushal M,et al. Diffusion tensor imaging in a large longitudinal series of patients with cervical spondylotic myelopathy correlated with long-term functional outcome[J]. Neurosurgery,2018,83(4):753-760.
[21] Dong F,Wu Y,Song P,et al. A preliminary study of 3.0-T magnetic resonance diffusion tensor imaging in cervical spondylotic myelopathy[J]. Eur Spine J,2018,27(8):1839-1845.