近年来,由于环境、食物和社会等诸多因素的影响,儿童性早熟的发病率呈逐年上升趋势[1-2]。性早熟按发病机制可分为中枢性性早熟(central precocious puberty,CPP)和外周性性早熟,在女孩中,80%以上的性早熟为特发性中枢性性早熟(idiopathic central precocious puberty,ICPP)[3]。单纯乳房早发育(premature thelarche,PT)和ICPP早期均表现为8岁之前乳房发育,但PT不伴有其他性发育的征象,仅需密切随访,无需特殊干预,而ICPP是一种以青春期发育提前、生长加速和骨龄快速成熟为特征的疾病[4]。在心智尚未成熟之前,第二性征早现往往会引起儿童青少年恐惧、自卑、焦虑等不良心理问题,甚至会带来社会问题和精神负担[5-6]。此外,由于线性生长提前和骨骺过早闭合,患者开始时往往身高较高,但成年后却较正常成人身高偏矮[7],需要促性腺激素释放激素类似物(gonadotrophin releasing hormone analogue,GnRHa)抑制发育,延缓骨骺闭合[8-9]。因此,对于ICPP早期诊断和鉴别诊断至关重要。迄今为止,ICPP的诊断仍以促性腺激素释放激素(gonadotropin releasing hormone,GnRH)激发试验作为“金标准”进行评价[10]。对于发育阶段的女童过早或过频的GnRH激发试验本身就是对发育的刺激。且此试验需要多次采血,检测时间长,程序繁琐,导致患儿依从性差。女孩青春期开始的标志是乳腺组织的发育,超声可排除脂肪组织等干扰,更准确的了解女孩乳腺和内生殖器的大小和结构,且无创、操作简单、费用低,更易被儿童及其父母接受[11]。乳腺超声分级与传统的临床 Tanner分期相比,可视化乳房的青春期发育阶段,并确保更准确的信息。盆腔超声已被应用于性早熟的诊断及鉴别诊断的过程[12-14],但乳腺超声并没有作为性早熟的主要参考依据。本研究旨在探讨乳腺和盆腔超声对ICPP的诊断价值。
1 资 料 与 方 法
1.1 一般资料 选取2016年1月—2018 年5月于河北大学附属医院门诊同时接受盆腔及乳腺超声检查以评价生长发育的女孩124 例为研究对象,年龄2.5~14.5岁,中位年龄8.9岁。对所有≤9岁的受试者进行回顾性诊断,54例女童在8岁前出现乳房发育,经GnRH激发试验及至少6个月随访,其中16例诊断为ICPP,38例诊断为PT,以上诊断符合2015年中枢性性早熟诊断与治疗共识[15]。
排除标准:①存在影响下丘脑-垂体-性腺轴的器质性疾病;②有慢性病史或特殊药物使用史;③临床、超声或骨龄及性激素等资料不完善;④第二性征发育顺序异常;⑤随访时间少于6个月。
1.2 方法
1.2.1 乳腺及盆腔超声 受试对象行超声检查前均饮水,使膀胱充分充盈,检查时取仰卧位,一名有经验的超声科医师操作Philips iu22型超声诊断仪,应用频率为10 MHz的探头,以乳头为中心,从顺/逆时针方向连续转动检查受试者乳房,存在乳房发育不对称时,以发育更明显的一侧乳头后低回声结节的的最长直径为乳芽直径(以cm为单位),乳芽体积=乳芽纵径×横径×前后径×0.523 3(以cm3为单位)。更换频率约7.5 MHz的探头,于下腹正中耻骨联合上方对受试者内生殖器进行测量与观察,子宫体积=子宫纵径×横径×前后径×0.523 3(以cm3为单位),卵巢体积以两侧卵巢中较大的一侧为准=卵巢纵径×横径×前后径×0.523 3(以cm3为单位),子宫厚/宫颈厚(uterus/anterior-posterior diameter of cervix,FCR)=子宫前后径/宫颈前后径。
1.2.2 乳腺超声分级 超声将乳房发育分5级[16-17]:①A级, 处于青春期前,乳晕后可见轻度不均匀组织,未见明显低回声结节;②B级,乳晕后可见直径<1 cm圆形,边缘呈线性的低回声结节(乳芽);③C级,乳晕后低回声结节(乳芽)增大,直径≥1 cm,伴或不伴有高回声腺体组织;④D级,乳晕周围高回声腺体组织及中央低回声结节进一步增大,且呈分枝状,伴皮下脂肪组织堆积;⑤E级,乳晕周围高回声腺体组织呈三角形伴皮下脂肪组织,无低回声中心结节(存在乳房不对称时,以发育更明显的一侧进行评估)。
1.2.3 临床、骨龄和性激素资料 由儿科内分泌医师测量并收集临床资料,身高测量脱鞋取直立平视位,体重测量时受试者脱鞋,穿轻便衣服。所有受试者的身高精确到0.1 cm、体重精确到0.1 kg,并计算体重指数(body mass index,BMI)=体重/身高2,骨龄采用G-P图谱法判读,精确到0.1岁,采用免疫化学发光法(immune chemiluminometric assay,ICMA)测定血清LH、FSH和E2值。结合54例在8岁前出现乳房发育女童的临床、超声、骨龄及基础性激素结果,对诊断不明确的受试者给予戈那瑞林激发试验[18],并进行至少6个月的随访。
1.3 统计学方法 应用SPSS 23.0统计软件分析数据。计量资料采用单因素方差分析、SNK-q检验、t检验(正态分布指标)或非参数检验(非正态分布指标),等级资料采用Kruskal-Wallis秩和检验。P<0.05为差异有统计学意义。
2 结 果
2.1 乳腺超声分级组间临床资料及超声参数 124例受试女童按乳腺超声分级,A级34例(27.4%)、B级49例(39.5%)、C级18例(14.5%)、D级5例(4%)、E级18例(14.5%)。比较5组间临床及超声参数的差异结果,见表1。受试者的年龄、BMI、子宫体积、骨龄、子宫长径、FCR值、最大卵巢体积、子宫内膜厚度、阴道壁厚度、≥4 mm卵泡数、最大卵泡直径、乳芽直径及乳芽体积各分级间差异均有统计学意义(P<0.05)。见表1。
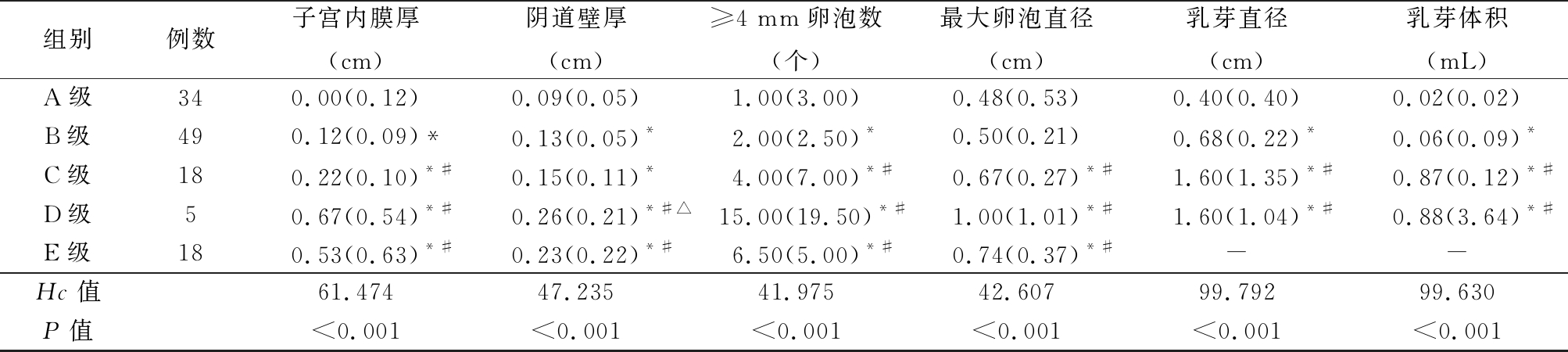
2.2 ICPP和PT女童的临床资料及超声参数 8岁前出现乳房发育的54例女童,经回顾性诊断,ICPP 16例,PT 38例,2组女童的临床及超声参数见表2。2组受试者年龄、子宫体积、子宫长径、子宫内膜厚度、最大卵巢体积、≥4 mm卵泡数、最大卵泡直径、乳芽直径及乳芽体积均存在统计学差异均有统计学意义(P<0.05),BMI、FCR值及阴道壁厚度差异均无统计意义(P>0.05)。2组女童的临床及超声参数见表2。
表1 乳腺超声分级的临床、盆腔超声和乳腺超声参数比较
Table 1 Comparison of clinical, pelvic and breast ultrasound parameters in different ultrasound grade of breast (M,QR)
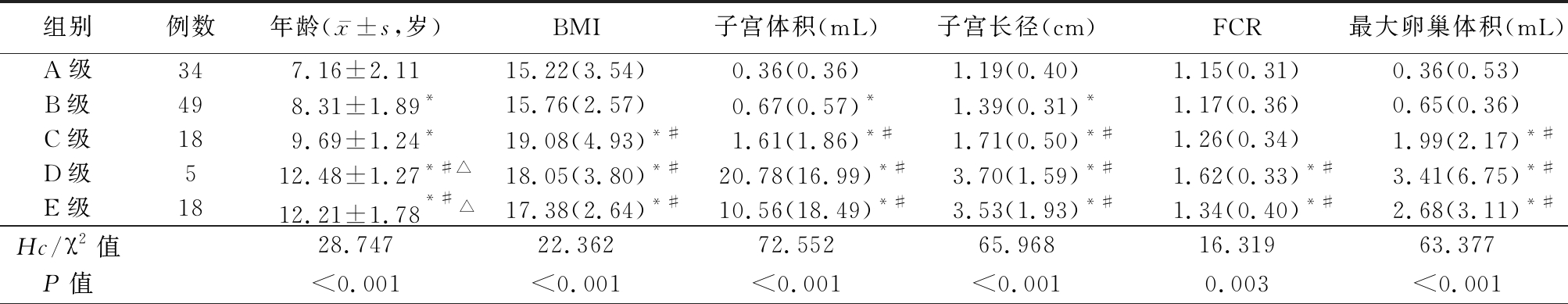
组别例数年龄(x-±s,岁)BMI子宫体积(mL)子宫长径(cm)FCR最大卵巢体积(mL)A级347.16±2.1115.22(3.54)0.36(0.36)1.19(0.40)1.15(0.31)0.36(0.53)B级498.31±1.89*15.76(2.57)0.67(0.57)*1.39(0.31)*1.17(0.36)0.65(0.36)C级189.69±1.24*19.08(4.93)*#1.61(1.86)*#1.71(0.50)*#1.26(0.34)1.99(2.17)*#D级512.48±1.27*#△18.05(3.80)*#20.78(16.99)*#3.70(1.59)*#1.62(0.33)*#3.41(6.75)*#E级1812.21±1.78*#△17.38(2.64)*#10.56(18.49)*#3.53(1.93)*#1.34(0.40)*#2.68(3.11)*#Hc/χ2值28.74722.36272.55265.96816.31963.377P值<0.001<0.001<0.001<0.0010.003<0.001
表1 (续)
*P值<0.05与A组比较 #P值<0.05与B组比较 △P值<0.05与C组比较(SNK-q检验) “-”表示未探及
组别例数子宫内膜厚(cm)阴道壁厚(cm)≥4 mm卵泡数(个)最大卵泡直径(cm)乳芽直径(cm)乳芽体积(mL)A级340.00(0.12)0.09(0.05)1.00(3.00)0.48(0.53)0.40(0.40)0.02(0.02)B级490.12(0.09)*0.13(0.05)*2.00(2.50)*0.50(0.21)0.68(0.22)*0.06(0.09)*C级180.22(0.10)*#0.15(0.11)*4.00(7.00)*#0.67(0.27)*#1.60(1.35)*#0.87(0.12)*#D级50.67(0.54)*#0.26(0.21)*#△15.00(19.50)*#1.00(1.01)*#1.60(1.04)*#0.88(3.64)*#E级180.53(0.63)*#0.23(0.22)*#6.50(5.00)*#0.74(0.37)*#--Hc值61.47447.23541.97542.60799.79299.630P值<0.001<0.001<0.001<0.001<0.001<0.001
表2 ICPP和PT女童临床、盆腔超声及乳腺超声参数比较
Table 2 Comparison of clinical, pelvic and breast ultrasound grades between ICPP and PT girls (M,QR)
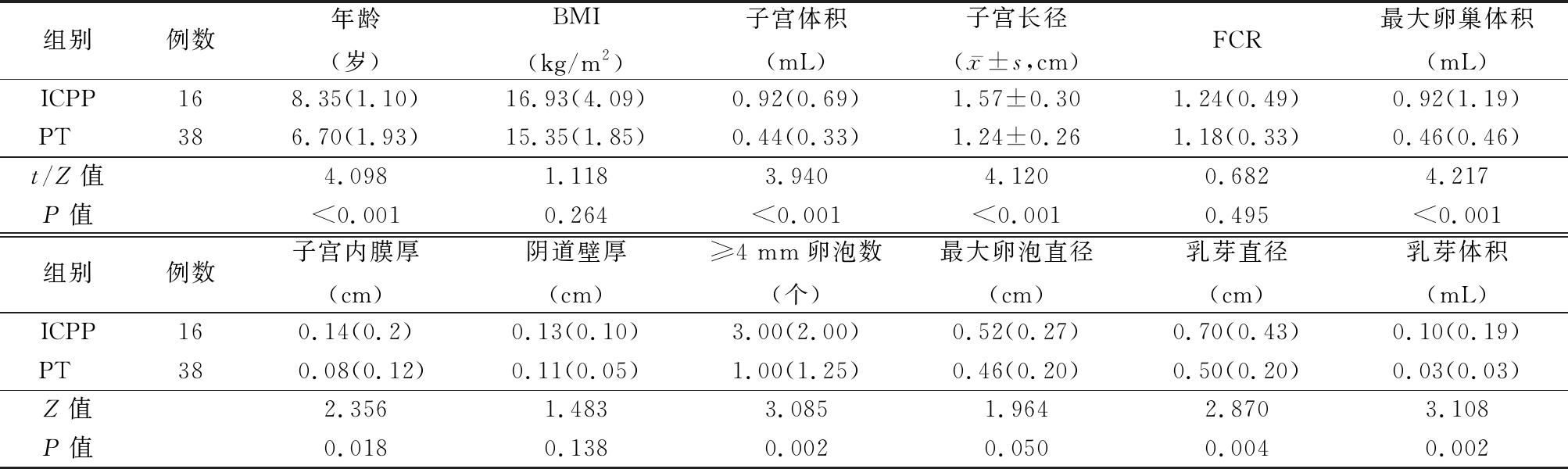
组别例数年龄(岁)BMI(kg/m2)子宫体积(mL)子宫长径(x-±s,cm)FCR最大卵巢体积(mL)ICPP168.35(1.10)16.93(4.09)0.92(0.69)1.57±0.301.24(0.49)0.92(1.19)PT 386.70(1.93)15.35(1.85)0.44(0.33)1.24±0.261.18(0.33)0.46(0.46)t/Z值4.0981.1183.9404.1200.6824.217P值<0.0010.264<0.001<0.0010.495<0.001组别例数子宫内膜厚(cm)阴道壁厚(cm)≥4 mm卵泡数(个)最大卵泡直径(cm)乳芽直径(cm)乳芽体积(mL)ICPP160.14(0.2)0.13(0.10)3.00(2.00)0.52(0.27)0.70(0.43)0.10(0.19)PT 380.08(0.12)0.11(0.05)1.00(1.25)0.46(0.20)0.50(0.20)0.03(0.03)Z值2.3561.4833.0851.9642.8703.108P值0.0180.1380.0020.0500.0040.002
2.3 ICPP和PT女童的乳腺超声分级 16例ICPP受试者按乳腺超声分级为:A级1例(6.3%),B级13例(81.2%),C级2例(12.5%) 。38例PT受试者乳腺超声分级为:中 A级18例(47.4%),B级18例(47.4%),C级2例(5.2%)。2组女童乳腺超声分级比较差异有统计学意义(Uc=7.906,P<0.05)。
3 讨 论
青春期是从儿童到成人的过渡期,是一个动态的、复杂的发育期,伴随着生长线性加速和性发育的成熟[19]。女性在性成熟过程中下丘脑-垂体-性腺激素轴被激活,引发GnRH脉冲式刺激垂体前叶分泌促性腺激素/促卵泡生成素和促黄体生成素[20],首先出现乳腺乳芽增大,腺体形成,其次才是卵巢及子宫的增大[21]。通过观察及简单触诊的Tanner分期可能不足以区分乳腺腺体及其周围组织。超声是一种简单、有效、无创的评价乳房状况的方法,Yüce等[17]首先提出了乳腺发育的超声分期,并依据乳芽的大小、形态及乳腺腺体组织是否存在确定了5个不同的乳腺发育阶段。对于肥胖儿童而言,超声乳腺发育分期较Tanner分期可提供更准确、更客观的数据。本次124例研究对象中只有14例(11%)BMI超出正常范围(3例超重,11例肥胖),但超声乳腺分级显示各级间子宫体积、子宫长径、子宫前后径/宫颈前后径比值、最大卵巢体积、子宫内膜厚度、阴道壁厚度、≥4 mm卵泡数、最大卵泡直径、乳芽直径及乳芽体积差异均存在统计学意义(P<0.05),且乳芽直径及乳房体积随着乳腺超声分级的进展而增加。本研究不仅通过超声对子宫、卵巢发育过程进行量化,而且通过乳芽直径及乳芽体积对乳房发育进行量化,进而对青春期发育分期做出准确及客观地评价,尤其是在临床查体不能确定时,超声可以作为有效地补充,更直观、定量地反应青春期发育过程中乳腺及内生殖器的动态变化。
女孩在8岁之前出现乳房发育,10岁之前月经初潮被定义为性早熟[15]。其中ICPP和PT都是以乳房发育为特征,很难仅以最初的表现进行区分,而二者对儿童的影响却有很大差异,所以早期区分ICPP和PT至关重要。Haber等[22]的研究表明盆腔超声可以用于8岁之前PT和ICPP女童的鉴别。Wen等[14]的研究也表明盆腔超声检查可用于鉴别性早熟女孩,且最佳鉴别参数随早熟形式和年龄间隔的不同而变化。虽然女童性早熟较男童更易被家长发现,但8岁后就医的儿童仍占了很大的比重,正常发育的女童在9岁之后开始出现子宫及卵巢的增大[23],然而发育进程后期治疗的价值远远低于青春期早期[24],所以本次研究既扩大了受试者的年龄范围,又兼顾诊断的价值,选取了54例符合性早熟定义的年龄≤9岁的女童,经回顾性诊断,ICPP 16例,PT 38例,2组受试者年龄、子宫体积、子宫长径、子宫内膜厚度、最大卵巢体积、≥4 mm卵泡数、最大卵泡直径差异均有统计学意义(P<0.05)。这与之前的研究结果一致,表明盆腔超声可以用于ICPP和PT的鉴别。
除了盆腔超声,研究还引入乳芽直径及乳芽体积,量化乳腺的发育状况。Calcaterra等[25]对快速进展型中枢性性早熟和非/缓慢进展型性早熟的研究表明,2组间乳腺体积及超声乳腺分级均存在差异,且乳腺体积≥为0.85 cm3是快速进展型中枢性性早熟的独立预测因素。这与本研究ICPP和PT 2组间乳芽体积、乳芽直径及乳腺超声分级均存在差异的研究结果相一致。其中ICPP组以B级分期为主(81.2%),而PT组A级和B级患儿数相同(均为47.4%),2组患儿乳腺超声分级的分布存在差异。但Youn等[26]的研究认为超声测量乳腺的乳芽直径和超声分级有助于评价乳腺的发育,但在鉴别乳房早熟和性早熟方面的应用有限,这可能也与其选取了2~8岁的受试人群有关。
本研究的局限性在于,这是一项回顾性研究,且研究对象的数量不足以确定乳腺超声分级中各阶段女孩子宫、卵巢、乳芽直径及乳腺体积的正常参考范围,对性早熟的研究主要集中在≤9岁的年龄段,且ICPP患儿数量较少,今后应进行更大规模的临床研究。
综上所述,超声是一种简便、无创、重复性,更容易被 ICPP 女孩及其父母接受的好方法。可以通过乳腺及盆腔超声对乳腺及内生殖器形态结构进行定量测定,尤其是在诊断不明确时,有助于更准确地评估青春期进程,并作为ICPP和PT的有效鉴别手段,为 ICPP 的诊断提供方便、客观的方法。
[1] Kaplowitz P,Bloch C. Evaluation and referral of children with signs of early puberty[J]. Pediatrics,2016,137(1):e20153732.
[2] Farello G,Altieri C,Cutini M,et al. Review of the literature on current changes in the timing of pubertal development and the incomplete forms of early puberty[J]. Front Pediatr,2019,7(5):147.
[3] Menon PS,Vijayakumar M. Precocious puberty--perspectives on diagnosis and management[J]. Indian J Pediatr,2014,81(1):76-83.
[4] Soriano-Guillén L,Argente J. Central precocious puberty,functional and tumor-related[J]. Best Pract Res Clin Endocrinol Metab,2019,690(19):30003-30005.
[5] Schagen SE,Cohen-Kettenis PT,Delemarre-van de Waal HA,et al. Efficacy and safety of gonadotropin-releasing hormone agonist treatment to suppress puberty in gender dysphoric adolescents[J]. J Sex Med,2016,13(7):1125-1132.
[6] Chen FR,Rothman EF,Jaffee SR. Early puberty,friendship group characteristics,and dating abuse in US girls[J]. Pediatrics,2017,139(6):e20162847.
[7] 吴韬,杜俊文,张坤,等.儿童矮小症485例病因探讨及治疗效果[J].河北医科大学学报,2018,39(12):1384-1388.
[8] Willemsen RH,Elleri D,Williams RM,et al. Pros and cons of GnRHa treatment for early puberty in girls[J]. Nat Rev Endocrinol,2014,10(6):352-363.
[9] Lin YC,Lin CY,Chee SY,et al. Improved final predicted height with the injection of leuprolide in children with earlier puberty:a retrospective cohort study[J]. PLoS One,2017,12(10):e0185080.
[10] Brito VN,Spinola-Castro AM,Kochi C,et al. Central precocious puberty: revisiting the diagnosis and therapeutic management[J]. Arch Endocrinol Metab,2016,60(2):163-172.
[11] Paesano PL,Colantoni C,Mora S,et al. Validation of an accurate and noninvasive tool to exclude female precocious puberty:pelvic ultrasound with uterine artery pulsatility index[J]. AJR Am J Roentgenol,2019,213(2):451-457.
[12] Yu HK,Liu X,Chen JK,et al. Pelvic ultrasound in diagnosing and evaluating the efficacy of gonadotropin-releasing hormone agonist therapy in girls with idiopathic central precocious puberty[J]. Front Pharmacol,2019,10(2):104.
[13] Binay C,Simsek E,Bal C. The correlation between GnRH stimulation testing and obstetric ultrasonographic parameters in precocious puberty[J]. J Pediatr Endocrinol Metab,2014,27(11/12):1193-1199.
[14] Wen X,Wen D,Zhang H,et al. Observational study pelvic ultrasound a useful tool in the diagnosis and differentiation of precocious puberty in Chinese girls[J]. Medicine(Baltimore),2018,97(10):e0092.
[15] 中华医学会儿科学分会内分泌遗传代谢学组,《中华儿科杂志》编辑委员会. 中枢性性早熟诊断与治疗共识(2015)[J].中华儿科杂志,2015,53(6):412-418.
[16] García CJ,Espinoza A,Dinamarca V,et al. Breast US in children and adolescents[J]. Radiographics,2000,20(6):1605-1612.
[17] Yüce Ö,Sevinç D. Ultrasonographic assessment of pubertal breast development in obese children: compliance with the clinic[J]. J Pediatr Endocrinol Metab,2018,31(2):137-141.
[18] 中华人民共和国卫生部. 性早熟诊疗指南(试行)[卫办医政发(195)号][J].中国儿童保健杂志,2011,19(4):390-392.
[19] Wood CL,Lane LC,Cheetham T. Puberty:normal physiology(brief overview)[J]. Best Pract Res Clin Endocrinol Metab,2019,33(19):101265.
[20] Kletter GB,Klein KO,Wong YY. A pediatrician's guide to central precocious puberty[J]. Clin Pediatr(Phila),2015,54(5):414-424.
[21] Sultan C,Gaspari L,Maimoun L,et al. Disorders of puberty[J]. Best Pract Res Clin Obstet Gynaecol,2018,48:62-89.
[22] Haber HP,Wollmann HA,Ranke MB. Pelvic ultrasonography: early differentiation between isolated premature thelarche and central precocious puberty[J]. Eur J Pediatr,1995,154(3):182-186.
[23] Ziereisen F,Guissard G,Damry N,et al. Sonographic imaging of the paediatric female pelvis[J]. Eur Radiol,2005,15(7):1296-1309.
[24] Wang M,Zhang Y,Lan D,et al. The efficacy of GnRHa alone or in combination with rhGH for the treatment of Chinese children with central precocious puberty[J]. Sci Rep,2016,6:24259.
[25] Calcaterra V,Sampaolo P,Klersy C,et al. Utility of breast ultrasonography in the diagnostic work-up of precocious puberty and proposal of a prognostic index for identifying girls with rapidly progressive central precocious puberty[J]. Ultrasound Obstet Gynecol,2009,33(1):85-91.
[26] Youn I,Park SH,Lim IS,et al. Ultrasound assessment of breast development: distinction between premature thelarche and precocious puberty[J]. AJR Am J Roentgenol,2015,204(3):620-624.