尿酸(uric acid,UA)是机体内嘌呤代谢的产物,血液中UA增多提示机体内UA的生成和(或)排泄出现了异常。随着生活水平的提高和生活方式的改变,我国的高尿酸血症(hyperuricemia,HUA)患者比例增高,正常人群中HUA总患病率从3.5%~25%[1-5],表明HUA已成为常见病。HUA一般指在正常嘌呤饮食状态下检测UA水平高于参考区间者,无症状HUA患者经常在常规体检化验时被检测发现,其表现为UA浓度增高,但未出现关节炎、肾结石等临床症状。早期HUA虽然没有症状,但是持续的HUA可以引发或伴发多种疾病。HUA的危害类似于高血压、糖尿病,除了可能引发痛风外, 与冠心病、高血压、糖尿病、高脂血症和脑卒中等有密切的关系。研究表明随着UA浓度的增加,代谢综合征[6]、糖尿病[7]、心血管病[8]风险明显增加,并且其浓度越高(每增加60 μmol/L,10 mg/L),代谢综合症和糖尿病发病率也越高[6,8]。我国对于UA分层与血糖(blood glucose,GLU)、血脂的关系研究较少,因此本研究将无症状HUA患者依据UA水平分成不同组别(以60 μmol/L为组距),分析不同浓度水平UA和GLU、血脂的关系。
1 资 料 与 方 法
1.1 一般资料 选择2017年2月—2018年10月在河北医科大学第二医院和河北省衡水市哈励逊国际和平医院进行正常体检的UA水平高于正常参考范围成年者4 918例为研究对象,其中男性2 741例,女性2 177例,年龄18~83岁,平均(43.13±12.23)岁。入选标准:本地居民;年龄18岁以上;查体前3 d正常饮食无暴饮暴食及饮酒;查体当天空腹抽血;未伴有其他任何严重的全身性疾病。排除标准:非汉族或伴有其他冠心病、脑卒中等其他重大全身疾病。
分组方法:以60 μmol/L为组距,依据UA浓度对男性、女性患者分别进行分组。男性以UA高于420 μmol/L (70.0 mg/L)为HUA,女性以UA高于360 μmol/L(60.0 mg/L)为HUA。男性患者分为四组,≤420 μmol/L为一组,2 195例,UA为(331.53±52.39)μmol/L;≤480 μmol/L为二组,373例,UA为(445.68±17.56)μmol/L;≤540 μmol/L为三组,122例,UA为(506.86±17.86)μmol/L;>540 μmol/L为四组,51例,UA为(594.92±66.59)μmol/L。女性患者分为三组,≤360 μmol/L为一组,2 064例,UA为(249.28±49.84)μmol/L;≤420 μmol/L为二组,83例,UA为(380.86±53.86)μmol/L;>420 μmol/L为三组,30例,UA为(463.07±46.52)μmol/L。
女性患者绝经前后UA有较大变化,其平均绝经年龄约为49岁[9],因此以49岁重新分组。≤49岁女性患者1 442例,≤360 μmol/L为一组,1 394例,UA为(243.93±48.55)μmol/L;UA>480 μmol/L的有5例,420~480 μmol/L的有8例,因例数太少,所以合并为>360 μmol/L组,为二组,48例,UA为(392.86±31.25)μmol/L。>49岁女性患者有735例,≤360 μmol/L为一组,670例,UA为(260.37±50.69) μmol/L;≤420 μmol/L为二组,43例,UA为(380.26±16.59)μmol/L;>420 μmol/L为三组,22例,UA为(467.96±52.60) μmol/L。
1.2 方法 所有体检者清晨空腹,UA、GLU测定应用罗氏cobas8000全自动生化分析仪,试剂为罗氏公司配套试剂,标准品和质控品均为罗氏公司产品,检测当日所有检测项目质控均在控。血脂指标选择三酰甘油(triglyceride,TG)、总胆固醇(total cholesterol,TC)、高密度脂蛋白(high-density lipoprotein,HDL)和低密度脂蛋白( low-density lipoprotein,LDL)。
1.3 统计学方法 应用SPSS 11.0统计软件分析数据。计量资料比较采用t检验和单因素方差分析。P<0.05为差异有统计学意义。
2 结 果
2.1 不同组别患者GLU和血脂的水平比较 男性患者随着UA浓度升高,TG、TC和LDL呈总体升高趋势,HDL呈总体下降趋势,差异有统计学意义(P<0.05),四组GLU浓度差异无统计学意义(P>0.05)。女性患者随着UA升高,GLU、TG、TC和LDL呈总体升高趋势,HDL呈总体下降趋势,差异有统计学意义(P<0.05)。见表1,2。
表1 男性患者组间GLU和血脂的水平比较
Table 1 Comparison of GLU and blood lipid levels in male patients ![]()
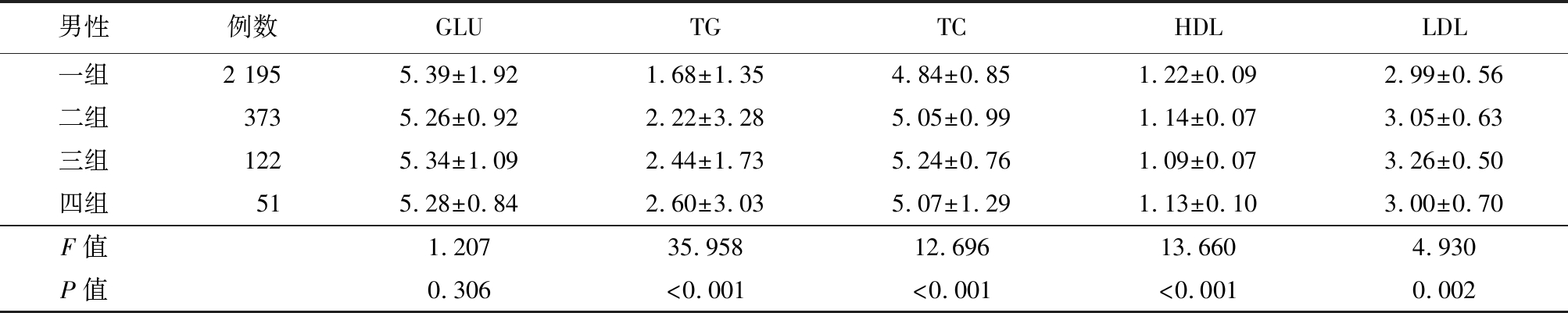
男性例数GLUTGTCHDLLDL一组2 1955.39±1.921.68±1.354.84±0.851.22±0.092.99±0.56二组 3735.26±0.922.22±3.285.05±0.991.14±0.073.05±0.63三组 1225.34±1.092.44±1.735.24±0.761.09±0.073.26±0.50四组 515.28±0.842.60±3.035.07±1.291.13±0.103.00±0.70F值1.20735.95812.69613.6604.930P值0.306<0.001<0.001<0.0010.002
表2 女性患者组间GLU和血脂的水平比较
Table 1 Comparison of GLU and blood lipid levels in female patients ![]()
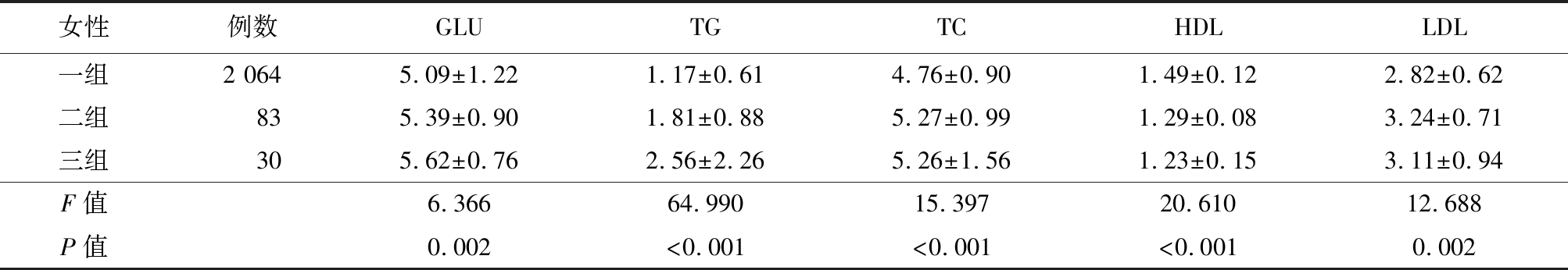
女性例数GLUTGTCHDLLDL一组2 0645.09±1.221.17±0.614.76±0.901.49±0.122.82±0.62二组 835.39±0.901.81±0.885.27±0.991.29±0.083.24±0.71三组 305.62±0.762.56±2.265.26±1.561.23±0.153.11±0.94F值6.36664.99015.39720.61012.688P值0.002<0.001<0.001<0.0010.002
2.2 49岁前后女性UA与GLU、血脂的关系 以49岁为分界,将女性分为不同组别后再依据UA水平进行分组,49岁以下女性人群随着UA升高,患者GLU、TG、TC、LDL升高,HDL降低,差异有统计学意义(P<0.05);49岁以上女性随着UA浓度升高,TG升高,HDL降低,差异有统计学意义(P<0.05),GLU、TC、LDL比较差异无统计学意义(P>0.05)。见表3,4。
表3 ≤49岁女性依据UA水平分组的患者血脂、血糖水平比较
Table 3 Comparison of blood lipid and blood glucose in women groups of ≤49 years based on UA level ![]()
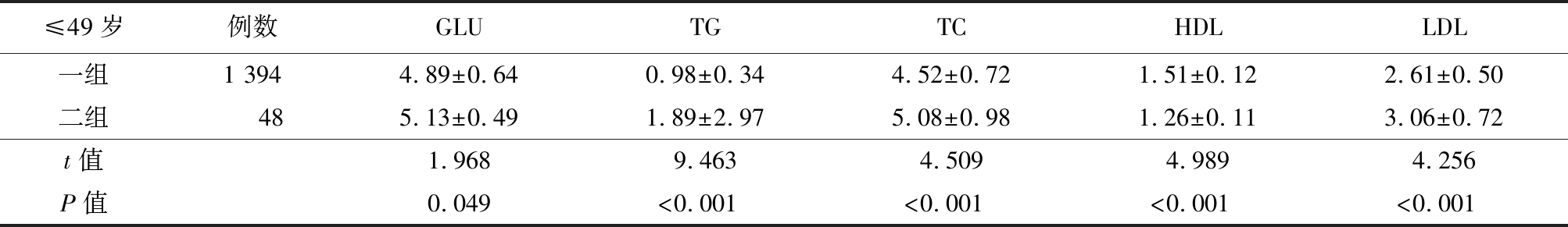
≤49岁例数GLUTGTCHDLLDL一组1 3944.89±0.640.98±0.344.52±0.721.51±0.122.61±0.50二组 485.13±0.491.89±2.975.08±0.981.26±0.113.06±0.72t值1.9689.4634.5094.9894.256P值0.049<0.001<0.001<0.001<0.001
表4 >49岁女性依据UA水平分组的患者血脂、血糖水平比较
Table 4 Comparison of blood lipid and blood glucose in women groups of >49 years based on UA level ![]()
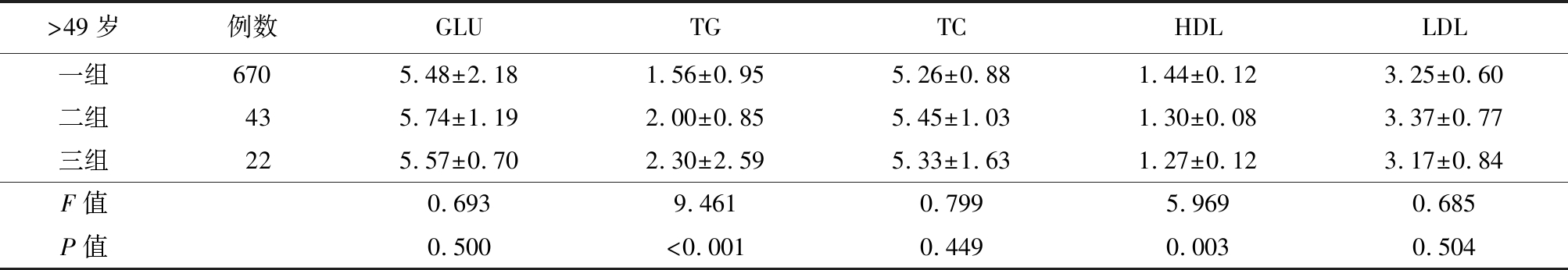
>49岁例数GLUTGTCHDLLDL一组6705.48±2.181.56±0.955.26±0.881.44±0.123.25±0.60二组435.74±1.192.00±0.855.45±1.031.30±0.083.37±0.77三组225.57±0.702.30±2.595.33±1.631.27±0.123.17±0.84F值0.6939.4610.7995.9690.685P值0.500<0.0010.4490.0030.504
3 讨 论
本研究结果显示,男性患者随着UA浓度升高,TG、TC和LDL呈总体升高趋势,HDL呈总体下降趋势(P<0.05),四组GLU浓度差异无统计学意义(P>0.05)。女性患者随着UA升高,GLU、TG、TC和LDL呈总体升高趋势,HDL呈总体下降趋势(P<0.05)。以49岁为分界,将女性分为不同组别后再依据UA水平进行分组,49岁以下女性人群随着UA升高,患者GLU、TG、TC、LDL升高,HDL降低(P<0.05);49岁以上女性随着UA浓度升高,TG升高,HDL降低(P<0.05),GLU、TC、LDL比较差异无统计学意义(P>0.05)。表明UA可能与脂类代谢密切相关,尤其是TG和HDL,与Osgood等[7]、You等[9]研究结果一致。Ryu等[10]在6年的随访调查后报道,TG浓度升高会提高HUA发病风险,而GLU和HDL则与HUA发病风险负相关。
近年来HUA作为代谢性疾病获得越来越多研究支持, Osgood等[7]研究结果表明UA浓度与血压、血脂和TC水平正相关,同时UA浓度也是胰岛素活性的预测因子,UA每升高60 μmol/L,胰岛素活性降低7.6%,UA浓度升高提示糖尿病风险增加。You等[9]在蒙古地区患者UA水平均与TG密切相关,UA浓度较高的患者代谢综合征的发生率也远远高于浓度较低的患者,同时其他相关疾病肥胖、高血压等发病率也增高。
由于机体构成和代谢的差异,女性人群的UA浓度远远低于男性人群,同时女性UA浓度还与激素水平有关,女性则绝经期前后UA浓度会有明显变化。Maruhashi等[11]研究显示对于女性而言,无论女性处于绝经前还是绝经后,TC、TG的浓度水平都与UA水平显著相关。以49岁为绝经分界线,对女性进行分组后再研究UA对女性患者血脂、GLU的影响[12-13]。本研究结果也表明激素对于女性UA的代谢有重要意义,而绝经前后UA与血脂、GLU的关系可能有一定差异,这需要更多的研究。
UA浓度升高与胰岛素抵抗、代谢综合征、心力衰竭、肾脏疾病等有关,UA影响血脂代谢的原因主要有几种可能,①高浓度UA可增加血管平滑肌细胞内活性氧的产生、激活肾素-血管紧张素系统、增加内皮素并刺激细胞内的氧化应激导致线粒体的改变和内皮一氧化氮的生物利用度减少;②UA代谢过程中的黄嘌呤氧化酶的激活诱导了血管内皮炎症以及后继氧化应激的发生,而黄嘌呤氧化酶抑制剂降低UA对机体产生的益处可能是由于阻断黄嘌呤氧化酶产生的氧化剂,而不是降低UA水平;③UA可能引发胰岛素抵抗,后者导致高胰岛素血症干扰脂质代谢,加重血脂代谢紊乱。而血脂代谢产生的酮体、游离的脂肪酸又会阻碍UA的排泄,使UA水平增高;另外HUA与血脂异常之间可能有某些遗传或获得性遗传共同缺陷,而UA对脂联素和瘦素也产生影响[14]。UA与血脂代谢及代谢综合征的关联需要更多的研究。
Raja等[15]认为高UA与生活方式和体重指数有关,并影响巴基斯坦人的身体健康,提出成年人群应该定期监测血UA水平。UA水平与多种疾病预后相关,慢性肾病进行血液透析的患者中,存在高UA血症患者心血管死亡率风险增加[16]。UA水平及对UA的治疗与心血管疾病的全因死亡率[13]有关。Sugano等[17]分析了高血UA血症与日本血液透析患者心血管疾病全因死亡率的关系,结果显示UA水平与这些患者全因死亡率和心血管死亡率相关,提出对HUA的干预可能会改善患者的预后。UA浓度升高与死亡率增加和临床不良反应相关,可作为心脏再同步治疗患者死亡率增加和临床不良反应的独立危险因子[18]。HUA患者糖尿病发病风险明显增加[19],即使是偶发性HUA患者在未来几年后发生糖尿病的风险明显增加。HUA的发病率在我国不同地区有不同报道,3.5%~25%[1-5],性别、高血压、高脂血症、饮酒、收缩压升高等为HUA
的危险因素[17],对无症状HUA血症患者的干预可能对糖尿病、高血压及其他代谢疾病产生积极影响[3,19]。
[1] 闫婕,陶慧,蒙健军,等.广西省南宁地区一常规体检人群高尿酸血症患病率调查及与血脂相关性的研究[J].中华内分泌代谢杂志,2014,30(5):411-414.
[2] 李少峰,陈燕董,陆玲,等.河北省张家口地区高尿酸血症流行现状及影响因素分析[J].医学动物防制,2018,34(5):455-457.
[3] 张磊,永建,焦丽亚,等.石家庄市40岁以上体检人群高尿酸血症患病率及危险因素分析[J].河北医科大学学报,2015,36(3):364-366.
[4] 陈蕾,伍成凯,康峻鸣,等.我国45岁及以上中老年人群高尿酸血症与常见慢性病的关联研究[J].中国全科医学,2021,24(4):447-452.
[5] 刘姝,徐开平,秦恳,等.成都地区高尿酸血症的患病情况及相关因素分析[J].西部医学,2012,24(3):474-476.
[6] Choi HK,Ford ES. Prevalence of the metabolic syndrome in individuals with hyperuricemia[J]. Am J Med,2007,120(5):442-447.
[7] Osgood K,Krakoff J,Thearle M. Serum uric acid predicts both current and future components of the metabolic syndrome[J]. Metab Syndr Relat Disord,2013,11(3):157-162.
[8] Kim SY,Guevara JP,Kim KM,et al. Hyperuricemia and coronary heart disease:a systematic review and meta-analysis[J]. Arthritis Care Res(Hoboken),2010,62(2):170-180.
[9] You L,Liu A,Wuyun G,et al. Prevalence of hyperuricemia and the relationship between serum uric acid and metabolic syndrome in the asian mongolian area[J]. J Atheroscler Thromb,2014,21(4):355-365.
[10] Ryu S,Chang Y,Zhang Y,et al. A cohort study of hyperuricemia in middle-aged South Korean men[J]. Am J Epidemiol,2012,175(2):133-143.
[11] Maruhashi T,Nakashima A,Soga J,et al. Hyperuricemia is independently associated with endothelial dysfunction in postmenopausal women but not in premenopausal women[J]. BMJ Open,2013,3(11):e003659.
[12] 周小会,汪丽杰,王科芳.2694例知识女性绝经年龄的调查分析[J].安徽医药,2012,16(2):206-207.
[13] Rasheed H,Hughes K,Flynn TJ,et al. Mendelian randomization provides no evidence for a causal role of serum urate in increasing serum triglyceride levels[J]. Circ Cardiovasc Genet,2014,7(6):830-837.
[14] Johnson RJ,S nchez-Lozada LG,Mazzali M,et al.What are the key arguments against uric acid as a true risk factor for hypertension[J].Hypertension,2013,61(5):948-951.
nchez-Lozada LG,Mazzali M,et al.What are the key arguments against uric acid as a true risk factor for hypertension[J].Hypertension,2013,61(5):948-951.
[15] Raja S,Kumar A,Aahooja RD,et al. Frequency of hyperuricemia and its risk factors in the adult population[J]. Cureus,2019,11(3):e4198.
[16] Petreski T,Ekart R,Hojs R,et al. Asymptomatic hyperuricemia and cardiovascular mortality in patients with chronic kidney disease who progress to hemodialysis[J]. Int Urol Nephrol,2019,51(6):1013-1018.
[17] Sugano N,Maruyama Y,Kidoguchi S,et al. Effect of hyperuricemia and treatment for hyperuricemia in Japanese hemodialysis patients:a cohort study[J]. PLoS One,2019,14(6):e0217859.
[18] Perge P,Boros AM,Zima E,et al. Hyperuricemia predicts adverse clinical outcomes after cardiac resynchronization therapy[J]. Scand Cardiovasc J,2018,52(5):250-255.
[19] Liu J,Tao L,Zhao Z,et al. Two-year changes in hyperuricemia and risk of diabetes:a five-year prospective cohort study[J]. J Diabetes Res,2018,2018:6905720.