宫颈癌是女性常见疾病,近年来发病率呈现逐渐升高趋势。研究指出,在我国宫颈癌乃女性第二大常见癌症,每年新发病例达10万左右[1]。宫颈癌早期患者多无明显临床症状及表现,少数出现不规则阴道出血及液体排出等[2]。因大部分患者早期无症状,早期诊断对患者预后具有重要意义。但宫颈癌疾病极为隐匿,其癌前病变期较长,根据研究指出,宫颈癌前病变最长可持续19年[3]。以往无论是对宫颈癌还是宫颈癌癌前病变进行诊断,多依靠病理检查,但该检查需切取宫颈组织,属于侵入性操作,部分患者无法接受。近年来,随着超声技术不断发展,经阴道彩色多普勒超声应用于早期宫颈癌诊断中已十分普遍。阴道超声可表现出宫颈管内部各细节,还可将血流状态进行展示,与阴道镜具有互补的效果[4]。本研究基于结合临床自身实践,选取宫颈癌及宫颈癌前病变患者90例作为研究对象,旨在分析经阴道彩色多普勒超声、阴道镜及两者联合诊断宫颈癌的价值,以期为临床早期诊断提供数据理论支持。现将研究结果报告如下。
1 资 料 与 方 法
1.1 一般资料 回顾性分析2018年1月—2019年12月河北省保定市第二中心医院收治的经病理诊断的早期宫颈癌患者62例及非宫颈癌患者28例(癌前病变19例、正常宫颈9例)的临床资料。宫颈癌患者年龄48~73岁,平均(61.58±10.66)岁;非宫颈癌患者年龄47~73岁,平均(61.80±10.63)岁。纳入标准:①临床资料完整,影像学资料图像清晰且齐全无缺失;②经病理诊断确诊;③存在性生活史,检查前3 d未发生过性关系或阴道冲洗等治疗。排除标准:①患有精神抑郁类疾病者或长期服用有关药物;②合并其他肿瘤或生殖系统疾病;③妊娠期产褥期女性。
1.2 检查方法
1.2.1 经阴道彩色多普勒超声检查 月经干净后择日检查,检查前24 h禁止进行阴道冲洗、用药及性生活。检查时采取仰卧位,嘱咐受试者放松,膀胱排空后防止涂抹耦合剂并将避孕套套至阴道探头处,小心送入阴道,进行纵向、横向及多方面检查。宫颈区主要对宫颈内口、外口宫颈管回声情况一级宫颈的整齐性进行观察;并对宫颈血流情况进行观察记录,包括收缩峰值期血流速度(peak systolic velocity,PsV)、阻力指数(resistance index,RI)。
1.2.2 阴道镜检查方法 月经干净后择日进行检查,检查前24 h禁止进行阴道冲洗、用药及性生活。检查时采取膀胱截石位,嘱咐受试者放松,常规外阴消毒后,放置窥阴器,以3%醋酸溶液涂抹宫颈,调整探头焦距后,放置阴道镜,显示屏放大宫颈图像并进行观察,成像最好时使用生理盐水进行冲洗,清理分泌物后,以复方碘液染色后于阴道镜模式下观察宫颈情况,查找异常影像特征。
1.3 观察指标 以患者病理检查结果作为金标准,比较经阴道彩色多普勒超声、阴道镜及两者联合对宫颈癌的诊断价值。并比较宫颈癌及非宫颈癌患者PSV、RI。
1.4 统计学方法 应用SPSS 22.0统计软件分析数据。计量资料比较采用单因素方差分析和SNK-q检验。阴道彩色多普勒超声、阴道镜对宫颈癌及癌前病变的诊断价值采用公式进行计算;采用Kappa一致性分析彩色多普勒超声、阴道镜及两者联合诊断与病理诊断结果的一致性,Kappa值≥0.75为一致性较高、0.4~0.74为一致性良好、<0.4为一致性差。P<0.05为差异有统计学意义。
2 结 果
2.1 彩色多普勒超声、阴道镜及两者联合与病理结果情况 彩色多普勒超声共检出宫颈癌61例、非宫颈癌29例,与病理结果比较Kappa系数为0.769;阴道镜共检出宫颈癌55例、非宫颈癌35例,与病理结果比较Kappa系数为0.588;两者联合共检出宫颈癌60例、非宫颈癌30例,与病理结果比较Kappa系数为0.949。见表1。
表1 阴道镜、阴道超声及两者联合与病理结果情况
Table 1 Colposcopy, transvaginal ultrasound and their combination with pathological results (n=90,例数)
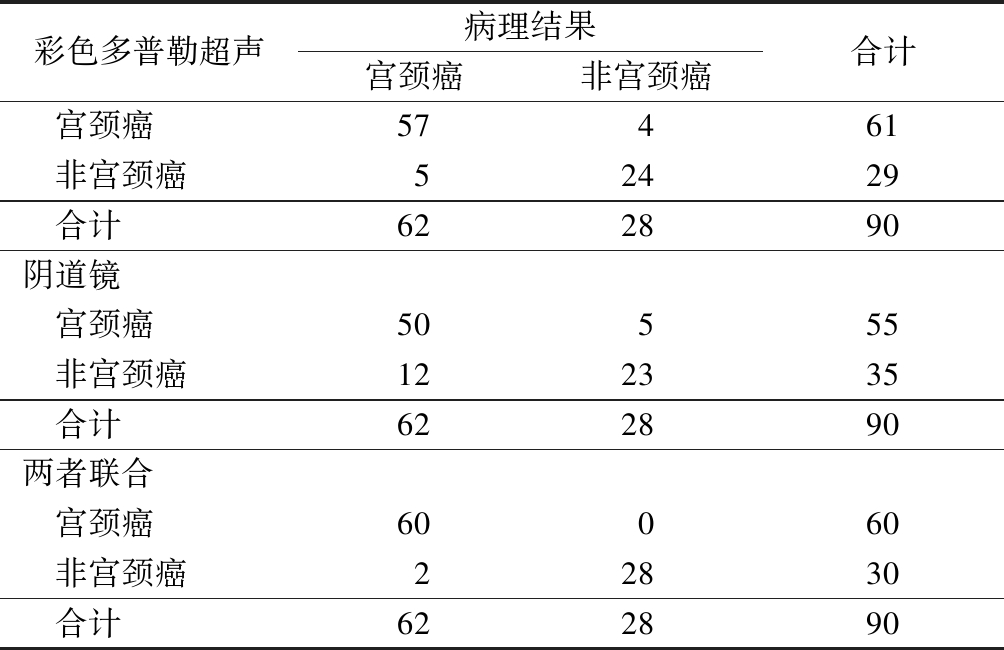
彩色多普勒超声病理结果宫颈癌非宫颈癌合计 宫颈癌57461 非宫颈癌52429 合计622890阴道镜 宫颈癌50555 非宫颈癌122335 合计622890两者联合 宫颈癌60060 非宫颈癌22830 合计622890
2.2 阴道彩色多普勒超声、阴道镜及两者联合诊断的价值 两者联合诊断宫颈癌的敏感度、特异度、阳性预测值、阴性预测值、诊断符合率均优于彩色多普勒超声、阴道镜单独诊断。见表2。
表2 阴道镜、阴道超声及两者联合的诊断价值
Table 2 Diagnostic value of colposcopy, transvaginal ultrasound and their combination (%)
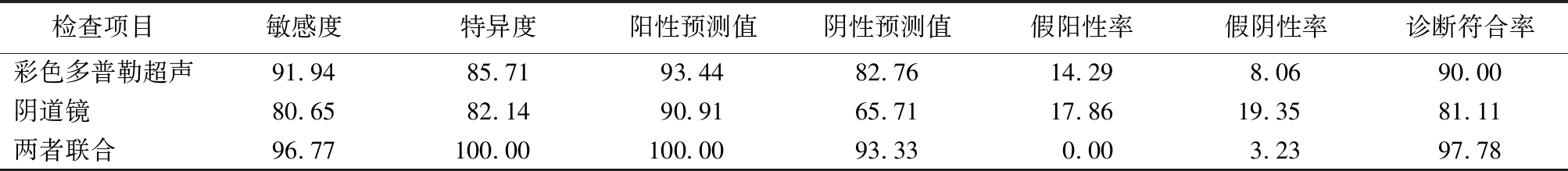
检查项目敏感度特异度阳性预测值阴性预测值假阳性率假阴性率诊断符合率彩色多普勒超声91.9485.7193.4482.7614.298.0690.00阴道镜 80.6582.1490.9165.7117.8619.3581.11两者联合 96.77100.00100.0093.330.003.2397.78
2.3 宫颈癌与癌前病变患者彩色多普勒超声参数比较 宫颈癌患者PSV显著低于癌前病变与正常宫颈,RI显著高于癌前病变与正常宫颈,差异有统计学意义(P<0.05)。见表3。
2.4 彩色多普勒超声参数对宫颈癌的ROC分析结果 PSV诊断宫颈癌的AUC为0.908,根据最佳临界值,敏感度为90.3%,特异度为85.7%。RI诊断宫颈癌的AUC为0.819,根据最佳临界值,敏感度为77.4%、特异度为67.9%。见表4,图1。
2.5 阴道彩色多普勒超声和阴道镜图片 宫颈癌中,阴道彩色多普勒超声可见宫颈增大,且内部存在低回声(图2)。阴道镜除癌前病变表现外,还可见镶嵌血管(图3)。
表3 宫颈癌与癌前病变患者彩色多普勒超声参数比较
Table 3 Comparison of color Doppler ultrasound parameters between cervical cancer and precancerous lesions![]()
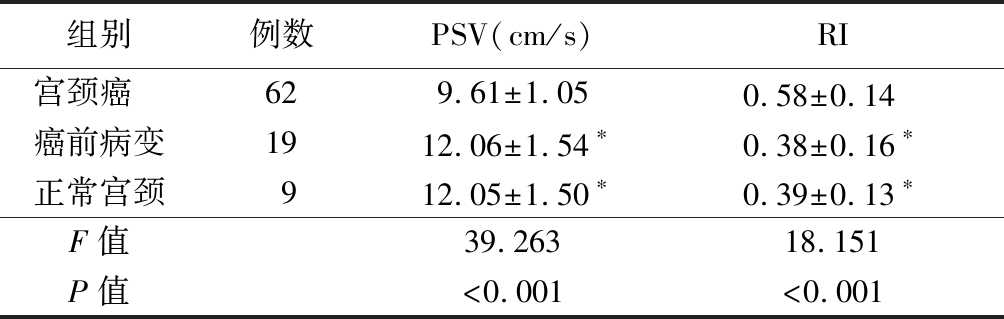
组别例数PSV(cm/s)RI宫颈癌 629.61±1.050.58±0.14 癌前病变1912.06±1.54∗0.38±0.16∗正常宫颈912.05±1.50∗0.39±0.13∗F值39.26318.151P值<0.001<0.001
*P值<0.05与宫颈癌比较(SNK-q检验)
表4 彩色多普勒超声参数对宫颈癌与癌前病变ROC分析结果
Table 4 ROC analysis of color Doppler ultrasound parameters for cervical cancer and precancerous lesions
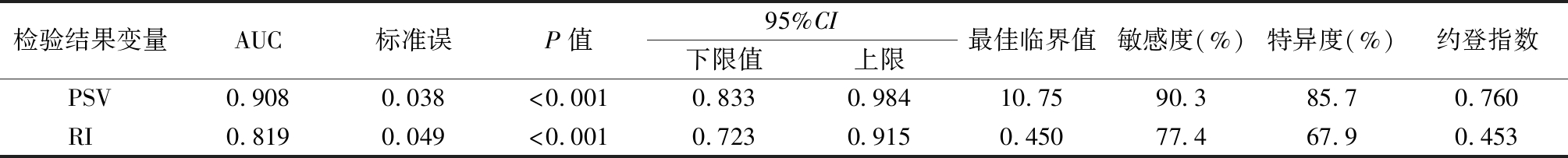
检验结果变量AUC标准误P值95%CI下限值上限最佳临界值敏感度(%)特异度(%)约登指数PSV0.9080.038<0.0010.8330.98410.7590.385.70.760RI 0.8190.049<0.0010.7230.9150.45077.467.90.453
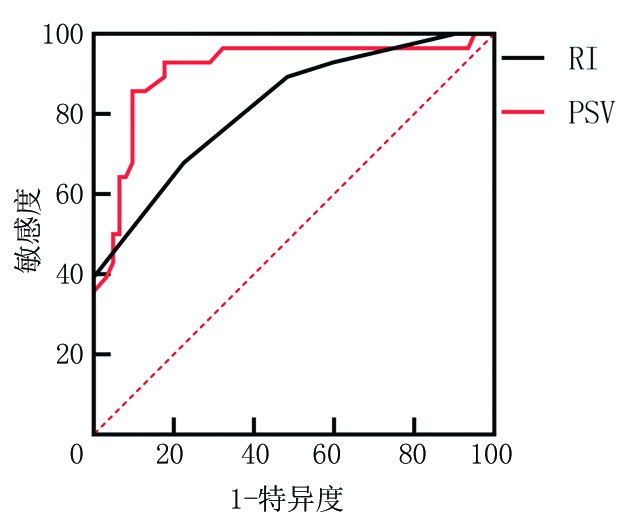
图1 PSV与RI诊断宫颈癌患者的ROC曲线图
Figure 1 ROC curve of PSV and RI in the diagnosis of a cervical cancer patient
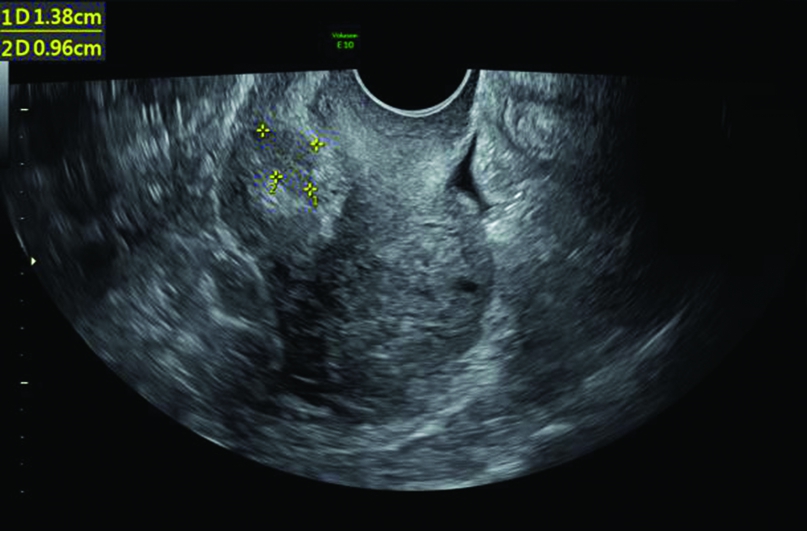
图2 宫颈癌患者阴道彩色多普勒超声图片
Figure 2 Image features of transvaginal color Doppler ultrasound of a cervical cancer patient

图3 宫颈癌患者阴道镜图片
Figure 3 Colposcopy image of a cervical cancer patient
3 讨 论
宫颈癌属于临床中常见的妇科肿瘤疾病,且结合临床统计结果观察,宫颈癌发生率呈现较快的增长速度[5-6]。临床中宫颈癌病情较为隐匿,确诊时大多已为中晚期,如何早期发现病变一直是医学界研究的重点[7-8]。目前,宫颈癌的主要诊断方式包括活体组织检查、阴道镜检查、经阴道镜彩色多普勒超声、宫颈刮片等。但上述检查中宫颈刮片与活体组织检查属于有创检查,部分患者无法接受。而阴道镜与经阴道彩色多普勒超声是国内外使用较多的检查方式,上述2种检查方法快速便捷,费用较低,重要的是不会造成创伤,因此在临床中得到广泛运用[9-10]。但研究[11-12]指出,经阴道彩色多普超声与阴道镜检查对宫颈癌出现一定误诊、漏诊率,主要因患者可能存在宫颈糜烂或宫颈炎症等表现导致。
本研究结果表明,阴道镜与彩色多普勒超声均出现一定的误诊及漏诊情况,其中彩色多普勒超声与病理结果Kappa系数为0.769,阴道镜与病理结果Kappa系数为0.588。这表明彩色多普勒超声诊断价值高于阴道镜检查。阴道镜主要通过显示屏显示工具结构,对宫颈内部进行解剖学关系进行观察,对周围组织黏连情况具有观察作用,同时通过碘制剂染色,了解宫颈癌病变范围,为临床医生提供疾病信息。但阴道镜存在一定的不足,阴道镜在为医师提供阴道镜图像时,医生可能带有自身主观性,若经验不足导致误诊、漏诊的概率较高[13]。另外,阴道镜观察期间需使用碘制剂,其染色范围与深度受到患者本身与药液发挥程度等因素的影响,在检查过程中极易因染色不合适导致无法观察到病变组织;此外阴道镜在区分宫颈癌与癌前病变上能力较差,本研究阴道镜与病理学一致性较低是最好的佐证[14]。彩色多普勒超声是近年来用于宫颈癌诊断的检查方法之一。研究[15]指出,经阴道彩色多普勒超声了解患者病灶内微血管血流情况,其血流越丰富获得的临床信息也越多。彩色多普勒超声不需要膀胱充盈,在实际操作中不受气体、体质量等因素影响,可清楚显示脏器解剖学机构,其探头频率较高,扫查视角也更为广泛,可对宫颈、阴道各个角落进行检查;最重要的是其能够评价病灶与周围血流动力学变化,这对手术治疗及宫颈癌与癌前病变提供了更多依据[16-17]。本研究中宫颈癌患者PSV指标显著低于癌前病变者与正常宫颈,RI高于癌前病变与正常宫颈,这提示彩色多普勒超声在宫颈癌与癌前病变、正常宫颈其血流程度存在明显差异;这有利于宫颈癌的诊断。
本研究结果显示,经阴道彩色多普勒超声联合阴道镜诊断宫颈癌敏感度为96.77%、特异度为100.0%,Kappa值为0.949。表明经阴道彩色多普勒超声联合阴道镜具有较高诊断价值,与病理结果一致性较高。这与多种研究结果一致[18]。经阴道彩色多普勒超声可了解患者病灶血流,与阴道镜结合后,能够起到相互弥补的作用,阴道镜无法探查区域,彩色多普勒超声可起到补充,阴道镜对宫颈结构可进行放大,可更好的发现微小病变[19]。
综上所述,经阴道彩色多普勒超声、阴道镜诊断宫颈癌均具有一定价值,但两者联合诊断价值更高,联合诊断可有效诊断宫颈癌,两者可起到相互弥补,相互协同的效果。
[1] 刘曼曼,李静,王金铭,等.高危型HPV阳性患者血清miRNA-26a表达水平对宫颈癌的预测价值[J].郑州大学学报(医学版),2019,54(5):696-699.
[2] 陈华,周措吉.ICAM-3、HIF-1蛋白表达水平与高原女性宫颈癌放疗抵抗的相关性研究[J].河北医科大学学报,2019,40(3):315-318,323.
[3] Jassim G,Obeid A,Al Nasheet HA. Knowledge,attitudes,and practices regarding cervical cancer and screening among women visiting primary health care centres in Bahrain[J]. BMC Public Health,2018,18(1):128-135.
[4] Akintomide A,Obasi U. Intimate patient examinations:the awareness,acceptance and practice preference of transvaginal ultrasound scan among women in a South-southern State of Nigeria[J]. J Family Med Prim Care,2019,8(1):109-114.
[5] 陈杰,李成,管建,等.阴道残端三维适形近距离补量放疗中膀胱容量的变化对正常器官受量的影响[J].实用临床医药杂志,2020,24(2):6-8.
[6] 邢海洋,张砚迪,王可心.基于SEER数据库分析放疗对宫颈癌患者生存的影响[J].实用临床医药杂志,2020,24(6):15-19.
[7] Liu M,Jia J,Wang X,et al. Long non-coding RNA HOTAIR promotes cervical cancer progression through regulating BCL2 via targeting miR-143-3p[J]. Cancer Biol Ther,2018,19(5):391-399.
[8] 沈洁,高丽丽,张月,等.北京市宫颈癌筛查妇女中高危型HPV感染状况及在宫颈癌前病变中的分布[J].中华预防医学杂志,2018,52(5):493-497.
[9] 赵爱珍,张小杉.经阴道彩色多普勒超声联合阴道镜检查对早期宫颈癌的诊断应用[J].内蒙古医科大学学报,2018,40(1):6-10.
[10] 孙明霞,蒋鹏程,于峰,等.经阴道彩色多普勒超声联合血清miRNA-18a和miRNA-92a诊断宫颈癌的价值研究[J].中国全科医学,2019,22(12):1436-1441.
[11] 胡素芝,叶咏菊.彩色多普勒超声检查早期宫颈癌病灶内微血管与患者临床病理特征、预后的关系[J].中国妇幼保健,2018,33(4):806-808.
[12] 龚芫,张惠民,芶飞飞,等.阴道镜在简化基层医院宫颈癌筛查步骤中的价值[J].中国医师杂志,2020,22(2):179-183.
[13] 屈海红,赵帅华,胡文娟.宫颈高危型HPV检测联合阴道镜检查对宫颈癌前病变的预测价值的前瞻性队列研究[J].实用癌症杂志,2018,33(12):2073-2076.
[14] 李云龙,韩风梅,李聪华.阴道镜及宫颈刮片细胞学在宫颈病变检查中的应用价值[J].医学动物防制,2016,32(12):1347-1349.
[15] 赵亮,刘宏.实时剪切波弹性成像与彩色多普勒超声在宫颈癌鉴别诊断中的应用价值[J].中国肿瘤临床与康复,2018,25(1):42-45.
[16] Wang HR,Lin Y,Zhang XY,et al. Transvaginal color doppler sonography combined with colposcopy for diagnosis of early stage cervical cancer and precancerous lesions[J]. J Biol Rregul Homeost Agents,2018,32(1):123-126.
[17] Wang P,Sun W,Wang L,et al. Correlations of p53 expression with transvaginal color Doppler ultrasound findings of cervical cancer after radiotherapy[J]. J BUON,2018,23(3):769-775.
[18] 孙海玲,陈凤兰,邓艳.彩色多普勒超声联合宫腔镜在宫内妊娠组织残留诊断和治疗中的临床价值[J].临床和实验医学杂志,2018,17(21):2334-2336.
[19] 卢永伟.阴道彩超联合阴道镜在早期宫颈癌病变诊断中的应用价值[J].中国当代医药,2018,25(35):50-52.