急性ST段抬高型心肌梗死(ST-segmentelevationmyocardialinfarction,STEMI)是由于冠状动脉内急性血栓形成引起管腔严重狭窄/闭塞,导致心肌缺血、坏死。直接经皮冠状动脉介入治疗(primary percutaneous coronary intervention,PPCI)是开通梗死相关动脉的最有效治疗措施。然而部分患者PPCI术中可出现血栓远端移位,导致微循环栓塞,出现慢血流/无复流,影响心肌组织灌注。血栓抽吸导管理论上可通过负压降低冠状动脉内血栓负荷,减少微循环栓塞,改善心肌灌注,从而改善临床预后[1]。但是,临床研究结果得出了不同的结论,全球心肌梗死工作组指南中多次调整血栓抽吸在PPCI中推荐级别,因此血栓抽吸导管在临床的应用仍存在较多的争议。本研究探讨在直接经皮冠状动脉介入治疗术中应用血栓抽吸对STEMI患者心肌灌注及临床预后的影响。
1 资料与方法
1.1 一般资料 采用回顾性研究方法,连续入选2017年2月—2019年2月于河北省人民医院胸痛中心行PPCI的STEMI患者446例。依据术中是否进行血栓抽吸将患者分为非血栓抽吸组(230例)和血栓抽吸组(216例)。入选标准:符合STEMI诊断标准[2];发病12 h以内;完成直接冠状动脉介入治疗。排除标准:非STEMI者;接受外周静脉溶栓治疗的STEMI者;未行PPCI或术中病死者;具有抗凝、抗血小板禁忌患者;合并肿瘤或其他系统严重疾病者。
本研究获得河北省人民医院医学伦理委员会批准。
1.2 PPCI及药物治疗 所有研究对象术前均签署冠状动脉介入治疗同意书,术前常规给予阿司匹林肠溶片300 mg和氯吡格雷300 mg/替格瑞洛180 mg嚼服,采用Seldinger法穿刺桡/股动脉行冠状动脉造影术,非血栓抽吸组只接受球囊扩张和(或)支架植入,血栓抽吸组支架植入术前先行血栓抽吸,其余手术操作两组一致。血栓抽吸过程按照冠状动脉血栓抽吸临床应用专家共识规范操作[3]。术中根据病情由术者决定是否应用血栓抽吸、替罗非班、尿激酶原、主动脉内球囊反搏(intra-aortic balloon pump,IABP)及支架植入数量。所有患者术中均接受普通肝素或比伐芦定抗凝治疗,术后应用低分子肝素抗凝1周。术后持续口服阿司匹林肠溶片100 mg/d和氯吡格雷75 mg/d或替格瑞洛180 mg/d至少12个月,结合患者具体情况术后及出院后给予他汀、血管紧张素转换酶抑制剂(angiotensin converting enzyme inhibitor,ACEI)、血管紧张素受体阻断剂(angiotensin ii receptor blockag,ARB)、β受体阻滞剂、尼可地尔等药物治疗。
1.3 分析指标 ①基线资料:年龄、性别、体重指数(body mass index, BMI)、冠心病史、高血压史、糖尿病史、高脂血症史、脑血管病史、家族史、吸烟史、是否前壁心肌梗死、Killip分级、院内用药情况、术后24 h内心脏超声射血分数;②冠状动脉手术资料:由经验丰富的介入医师完成,包括入院至球囊扩张时间(door to balloon time,D2B)时间、总缺血时间、手术入路、造影剂用量、是否多支病变、靶血管、血栓负荷、术前及术后心肌梗死溶栓实验(thrombolysis in myocardial infraction,TIMI)血流分级、是否应用IABP、支架植入数量、校正的TIMI血流帧数(corrected TIMI frame count,cTFC);③相关指标定义:TIMI血栓分级:0级,冠状动脉造影未见血栓影;1级,冠状动脉造影示管腔显影模糊、云雾影、病变轮廓不规则或完全闭塞部位突出管腔的平滑新月形影像,可疑血栓;2级,明确存在血栓,血栓长度≤1/2血管直径;3级,明确存在血栓,血栓长度为血管直径的1/2~2倍;4级,明确存在血栓,血栓长度≥2倍的血管直径;5级,血栓形成导致管腔完全闭塞。冠状动脉造影显示冠状动脉血栓负荷≥4级定义为高血栓负荷人群。无复流定义为TIMI血流0~1级;慢血流定义为PCI术中TIMI血流0、1、2及术后最终cTFC>40帧。
1.4 随访观察 所有研究对象均接受至少12个月的电话或门诊随访,包括危险因素的控制、出院后用药情况及是否发生主要不良心血管事件(major adverse cardiovascular events,MACE)和新发缺血性脑卒中事件,MACE事件包括心原性死亡、再发心肌梗死、靶血管血运重建。
1.5 统计学方法 应用SPSS 22统计软件处理数据。符合正态分布的计量资料比较采用独立样本t检验;非正态分布的计量资料比较采用Mann-Whitney秩和检验。计数资料比较采用χ2检验、Fisher精确概率法。采用多因素二元Logistic回归分析血栓抽吸对于术后慢血流/无复流影响,研究对象的临床事件的生存曲线采用Kaplan-Meier分析,组间比较采用Log-Rank检验。MACE事件及心原性死亡的多因素分析采用Cox回归分析。P<0.05为差异有统计学意义。
2 结 果
2.1 两组临床基线资料的比较 与非血栓抽吸组相比,血栓抽吸组造影显示TIMI血栓负荷≥4级、术前TIMI血流<3级及术中替罗非班、尿激酶原的使用率更高,术中造影剂用量更多,而多支病变的比率较低,差异有统计学意义(P<0.05)。其余临床基线资料包括年龄、性别、危险因素、冠状动脉病变指标及用药情况两组差异均无统计学意义(P>0.05)。见表1。
表1 研究对象临床基线资料比较
Table 1 Comparison of baseline, clinical and medical treatment characteristics between groups
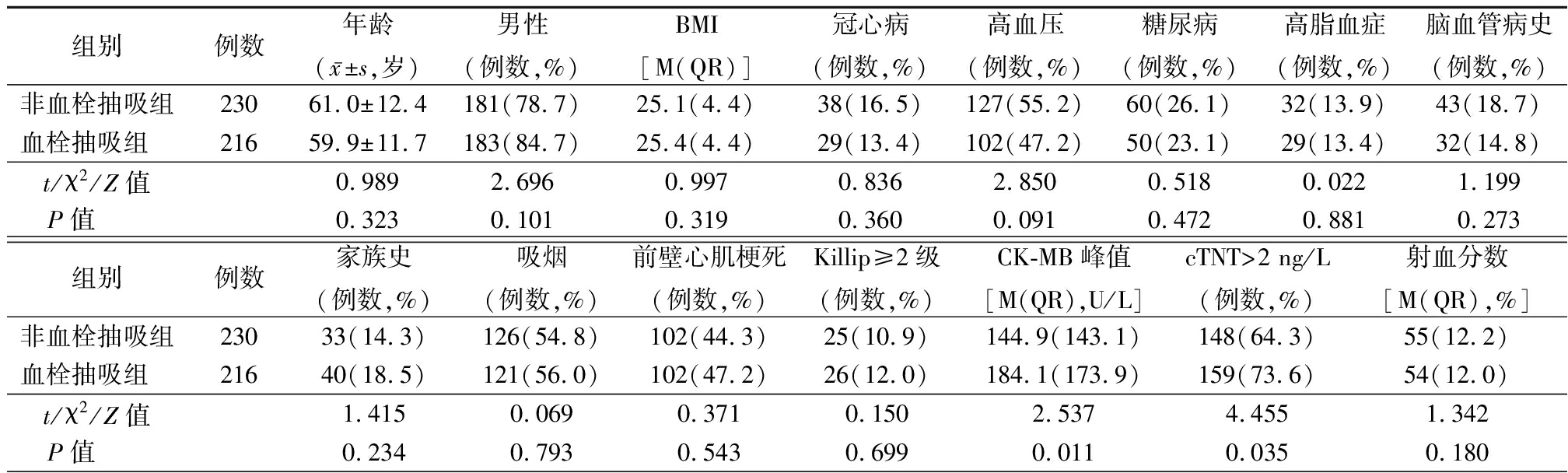
组别例数年龄(x-±s,岁)男性(例数,%)BMI[M(QR)]冠心病(例数,%)高血压(例数,%)糖尿病(例数,%)高脂血症(例数,%)脑血管病史(例数,%)非血栓抽吸组23061.0±12.4181(78.7)25.1(4.4)38(16.5)127(55.2)60(26.1)32(13.9)43(18.7)血栓抽吸组 21659.9±11.7183(84.7)25.4(4.4)29(13.4)102(47.2)50(23.1)29(13.4)32(14.8)t/χ2/Z值0.9892.6960.9970.8362.8500.5180.0221.199P值 0.3230.1010.3190.3600.0910.4720.8810.273组别例数家族史(例数,%)吸烟(例数,%)前壁心肌梗死(例数,%)Killip≥2级(例数,%)CK-MB峰值[M(QR),U/L]cTNT>2 ng/L(例数,%)射血分数[M(QR),%]非血栓抽吸组23033(14.3)126(54.8)102(44.3)25(10.9)144.9(143.1)148(64.3)55(12.2)血栓抽吸组 21640(18.5)121(56.0)102(47.2)26(12.0)184.1(173.9)159(73.6)54(12.0)t/χ2/Z值1.4150.0690.3710.1502.5374.4551.342P值 0.2340.7930.5430.6990.0110.0350.180
表1 (续)
组别例数用药情况(例数,%)阿司匹林替格瑞洛他汀ACEI/ARBβ受体阻滞剂螺内酯硝酸酯尼可地尔非血栓抽吸组230230(100.0)174(75.7)215(93.5)175(76.1)189(82.2)174(75.7)87(37.8)101(43.9)血栓抽吸组 216216(100.0)173(80.2)208(96.3)153(70.8)171(79.2)176(81.5)50(23.1)79(36.6)t/χ2/Z值-1.2721.8091.5800.6472.24111.2762.492P值 -0.2590.1790.2090.4210.1340.0010.114组别例数D2B时间[M(QR),min ]总缺血时间[M(QR),h]股动脉入路(例数,%)造影剂用量[M(QR),mL]多支病变(例数,%)非血栓抽吸组23061.5(9.8)3.00(2.5)34(14.8)130(70)180(78.3)血栓抽吸组 21661.0(12.0)3.00(3.0)40(18.5)140(40)154(71.3)t/χ2/Z值0.1780.7211.1233.0422.873P值 0.8590.4710.2890.0020.090组别例数靶血管(例数,%)前降支回旋支右冠状动脉左主干血栓负荷≥4级(例数,%)术前TIMI<3级(例数,%)IABP(例数,%)非血栓抽吸组230105(45.7)32(13.9)88(38.3)5(2.2)144(62.6)177(77.0)4(1.7)血栓抽吸组 216102(47.2)22(10.2)90(41.7)2(0.9)196(90.7)206(95.4)8(3.7)t/χ2/Z值1.06748.65631.1361.642P值 0.785<0.001<0.0010.200组别例数DES≥2个(例数,%)术后cTFC[M(QR),帧]慢血流/无复流(例数,%)普通肝素(例数,%)替罗非班(例数,%)尿激酶原(例数,%)非血栓抽吸组23036(15.7)25(20.0)53(23.0)190(82.6)60(26.1)13(5.7)血栓抽吸组 21636(16.7)25(18.0)43(19.9)179(82.9)95(44.0)78(36.1)t/χ2/Z值0.0850.9550.6490.00515.73063.632P值 0.7710.3400.4210.942<0.001<0.001
二元Logistic回归分析显示造影TIMI血栓负荷≥4级(OR=3.827,95%CI:1.995~7.339,P<0.001)、术前TIMI血流<3级(OR=2.650,95%CI:1.115~6.297,P=0.027)是PPCI术中使用血栓抽吸的影响因素(P<0.05)。
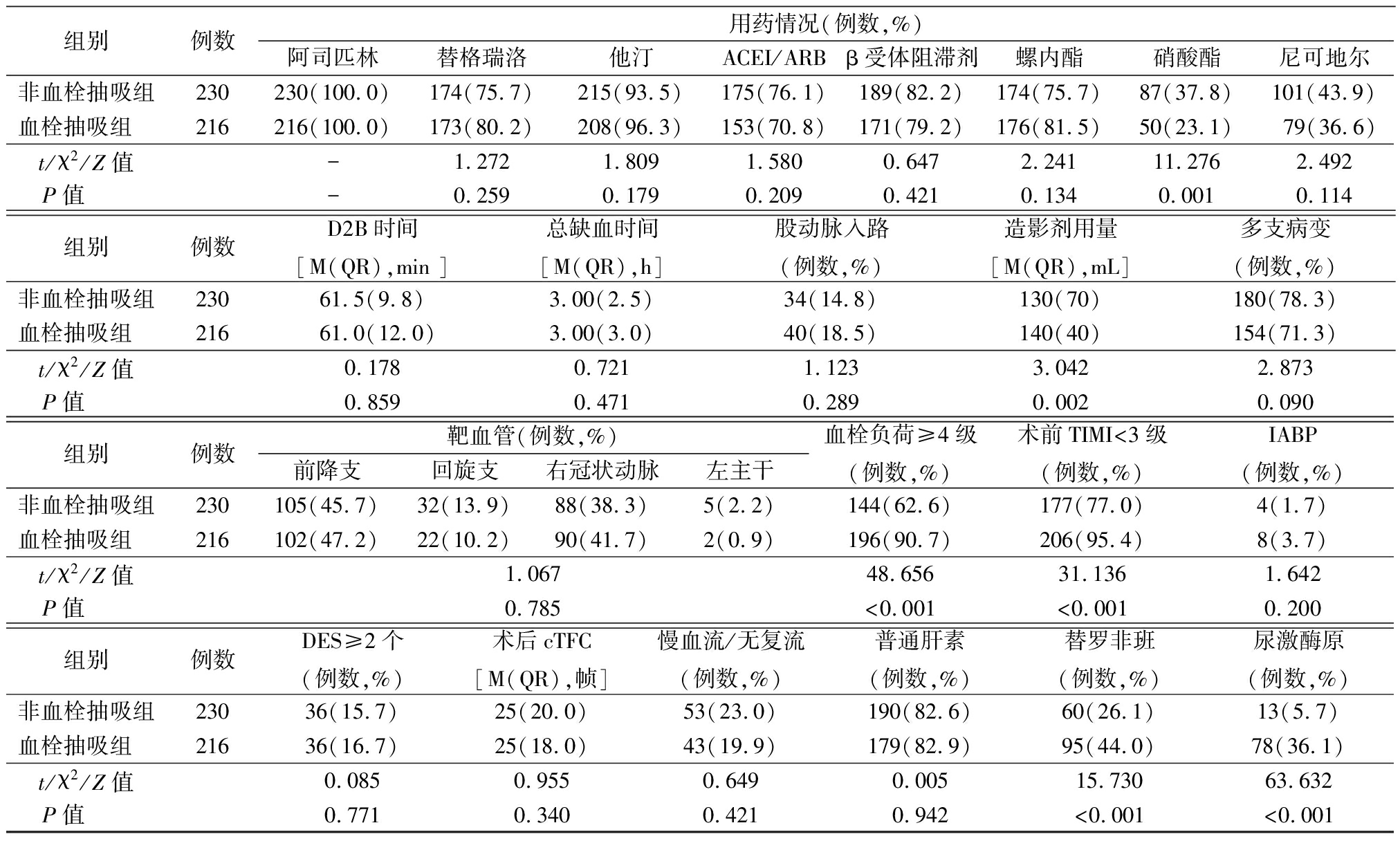
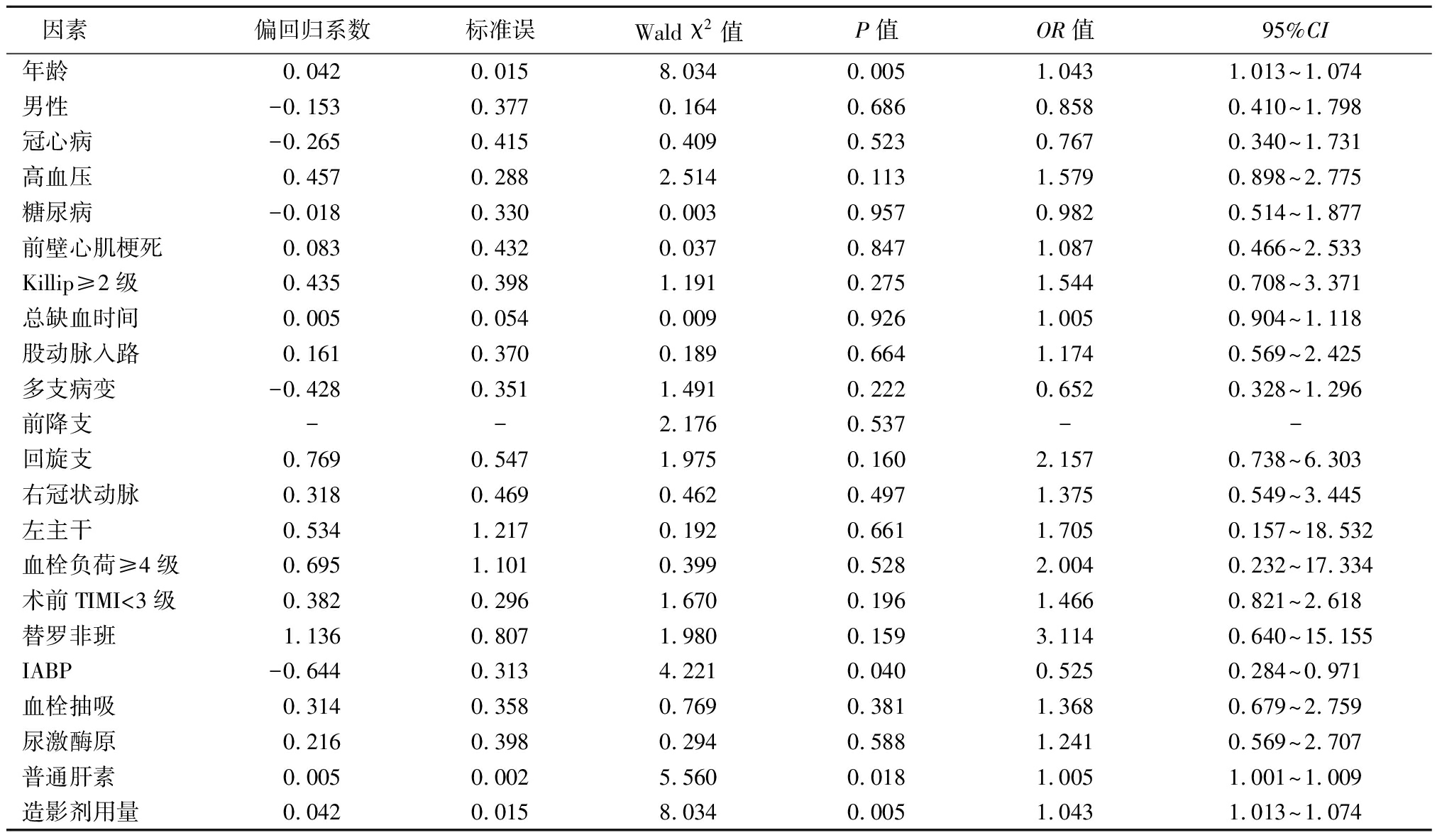
2.2 血栓抽吸对PPCI术后慢血流/无复流影响 以术后发生慢血流/无复流为因变量,以年龄(连续性变量)、性别(女性=0,男性=1)、冠心病(无=0,有=1)、高血压(无=0,有=1)、糖尿病(无=0,有=1)、前壁心肌梗死(无=0,有=1)、Killip≥2级(无=0,有=1)、总缺血时间、股动脉入路(无=0,有=1)、多支病变(无=0,有=1)、靶血管(前降支=1,回旋支=2,右冠脉=3,左主干=4)、血栓负荷是否≥4级(无=0,有=1)、造影TIMI血流<3级(无=0,有=1)、替罗非班(无=0,有=1)、尿激酶原(无=0,有=1)、术中抗凝(比伐芦定=0,普通肝素=1)、IABP(无=0,有=1)、血栓抽吸(无=0,有=1)、造影剂用量为自变量,行多因素二元Logistic回归分析(表2),结果显示:年龄(OR=1.03,95%CI:1.004~1.056,P=0.023)、造影剂用量(OR=1.004,95%CI:1~1.008,P=0.047)是发生无复流的独立危险因素;发生慢血流/无复流组患者较正常血流组患者中术中行血栓抽吸的比率低(44.8% vs. 49.4%),多因素分析显示在全体人群中血栓抽吸(OR=0.590,95%CI:0.338~1.031,P=0.064)与慢血流/无复流无关。
表2 直接冠状动脉介入治疗术后慢血流/无复流相关因素二元Logistic回归分析
Table 2 Logistic regression analysis of the related factors of slow flow/no-reflow after PPCI
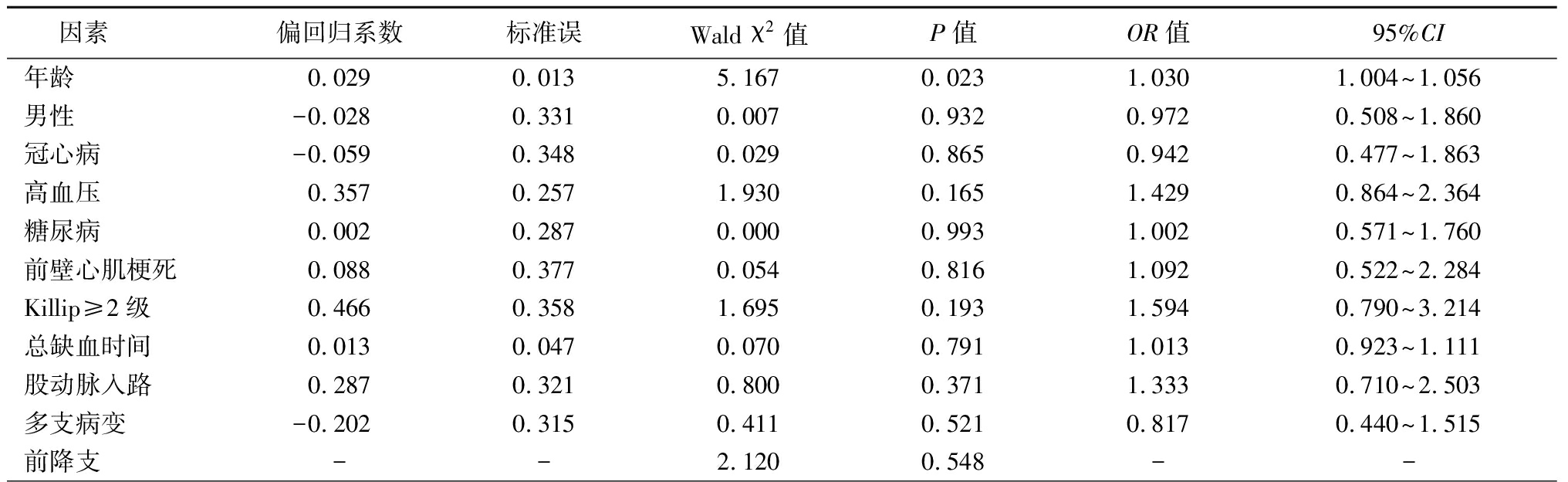
因素 偏回归系数标准误Wald χ2值P值OR值95%CI年龄0.0290.0135.1670.0231.0301.004~1.056男性-0.0280.3310.0070.9320.9720.508~1.860冠心病-0.0590.3480.0290.8650.9420.477~1.863高血压0.3570.2571.9300.1651.4290.864~2.364糖尿病0.0020.2870.0000.9931.0020.571~1.760前壁心肌梗死0.0880.3770.0540.8161.0920.522~2.284Killip≥2级0.4660.3581.6950.1931.5940.790~3.214总缺血时间0.0130.0470.0700.7911.0130.923~1.111股动脉入路0.2870.3210.8000.3711.3330.710~2.503多支病变-0.2020.3150.4110.5210.8170.440~1.515前降支--2.1200.548--
表2 (续)
回旋支0.6890.4832.0380.1531.9920.773~5.133右冠状动脉0.4500.4051.2340.2671.5680.709~3.469左主干-0.0651.0720.0040.9520.9370.115~7.669血栓负荷≥4级0.3500.3990.7710.3801.4190.650~3.100术前TIMI<3级0.6980.5311.7260.1892.0100.709~5.693替罗非班0.4340.2642.7070.1001.5440.920~2.591IABP0.9340.7631.5000.2212.5440.571~11.34血栓抽吸-0.5270.2843.4350.0640.5900.338~1.031尿激酶原0.1380.3330.1710.6791.1480.597~2.207普通肝素-0.1200.3510.1160.7330.8870.446~1.765造影剂用量0.0040.0023.9560.0471.0041.000~1.008
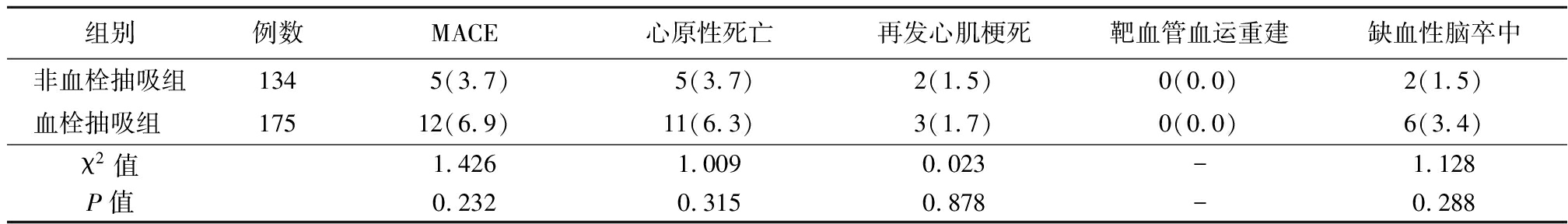
2.3 临床随访资料 446例STEMI患者中共有401例完成随访,其中非血栓抽吸组随访率为92.3%(212/230),血栓抽吸组随访率为87.5%(189/216)。非血栓抽吸组随访时间为21(11.5)个月,血栓抽吸组随访时间为24(15.5)个月。两组术后12个月的MACE、心原性死亡、再发心肌梗死、靶血管重建及缺血性脑卒中发生率差异无统计学意义(P>0.05)。见表3。Kaplan-Meier生存分析比较两组术后12个月无MACE(Log-Rank=0.274,P=0.601)、心原性死亡的累计生存率(Log-Rank=0.947,P=0.331),差异均无统计学意义(P>0.05)。
表3 直接冠状动脉介入治疗术后12个月随访的临床预后比较
Table 3 Comparison of clinical prognosis at 12-month follow-up between groups (例数,%)
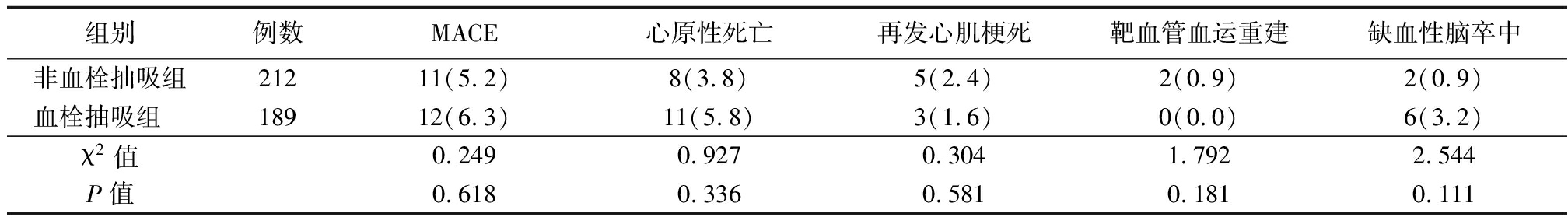
组别例数MACE心原性死亡再发心肌梗死靶血管血运重建缺血性脑卒中非血栓抽吸组21211(5.2)8(3.8)5(2.4)2(0.9)2(0.9)血栓抽吸组 18912(6.3)11(5.8)3(1.6)0(0.0)6(3.2)χ2值0.2490.9270.3041.7922.544P值0.6180.3360.5810.1810.111
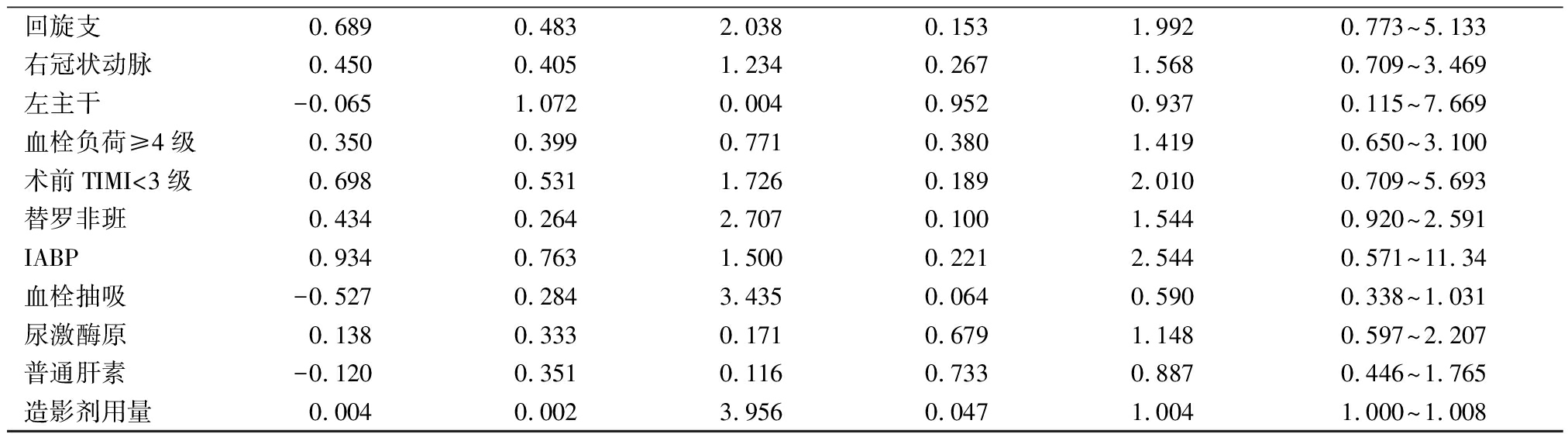
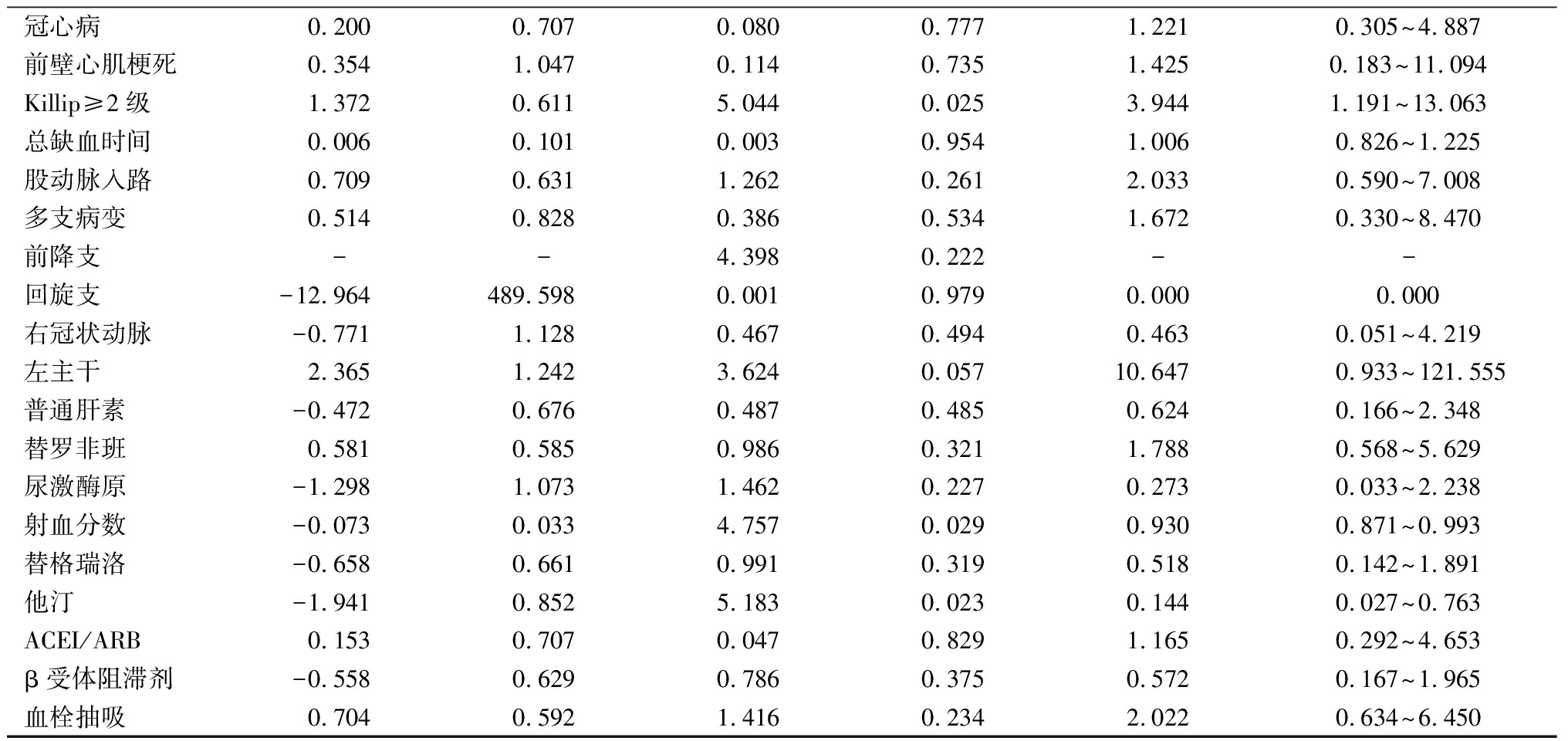
2.4 Cox回归分析结果 分别以术后12个月内是否发生MACE为因变量,以年龄(连续性)、性别(女性=0,男性=1)、冠心病(无=0,有=1)、前壁心梗(无=0,有=1)、Killip≥2级(无=0,有=1)、总缺血时间、手术入路(桡动脉=0,股动脉=1)、多支病变(无=0,有=1)、靶血管前降支=1,回旋支=2,右冠状动脉=3,左主干=4)、血栓抽吸(无=0,有=1)、术中普通肝素抗凝(无=0,有=1)、替罗非班(无=0,有=1)、尿激酶原(无=0,有=1)、院内射血分数及院内外应用药物,包括替格瑞洛(无=0,有=1)、他汀(无=0,有=1)、ACEI/ARB(无=0,有=1)、β受体阻滞剂(无=0,有=1)为自变量,进行多因素Cox回归分析,结果显示:Killip≥2级(HR=3.118,95%CI:1.099~8.844,P=0.033)和左主干病变(HR=13.410,95%CI:1.707~105.341,P=0.014)是MACE的独立危险因素,而他汀类药物(HR=0.218,95%CI:0.050~0.947,P=0.042)是MACE的保护性因素;Killip≥2级(HR=3.944,95%CI: 1.191~13.063,P=0.025)是心原性死亡的独立危险因素,而他汀类药物(HR=0.144,95%CI:0.027~0.763,P=0.023)和射血分数(HR=0.93,95%CI: 0.871~0.993,P=0.029)是心原性死亡的保护性因素。血栓抽吸与术后12个月MACE、心原性死亡的发生无关(P>0.05)。见表4。
表4 STEMI患者PPCI术后12个月发生MACE的多因素Cox回归分析
Table 4 Multivariate Cox regression analysis of the predictors of MACE during 12-month follow-up
after PPCI for STEMI patients
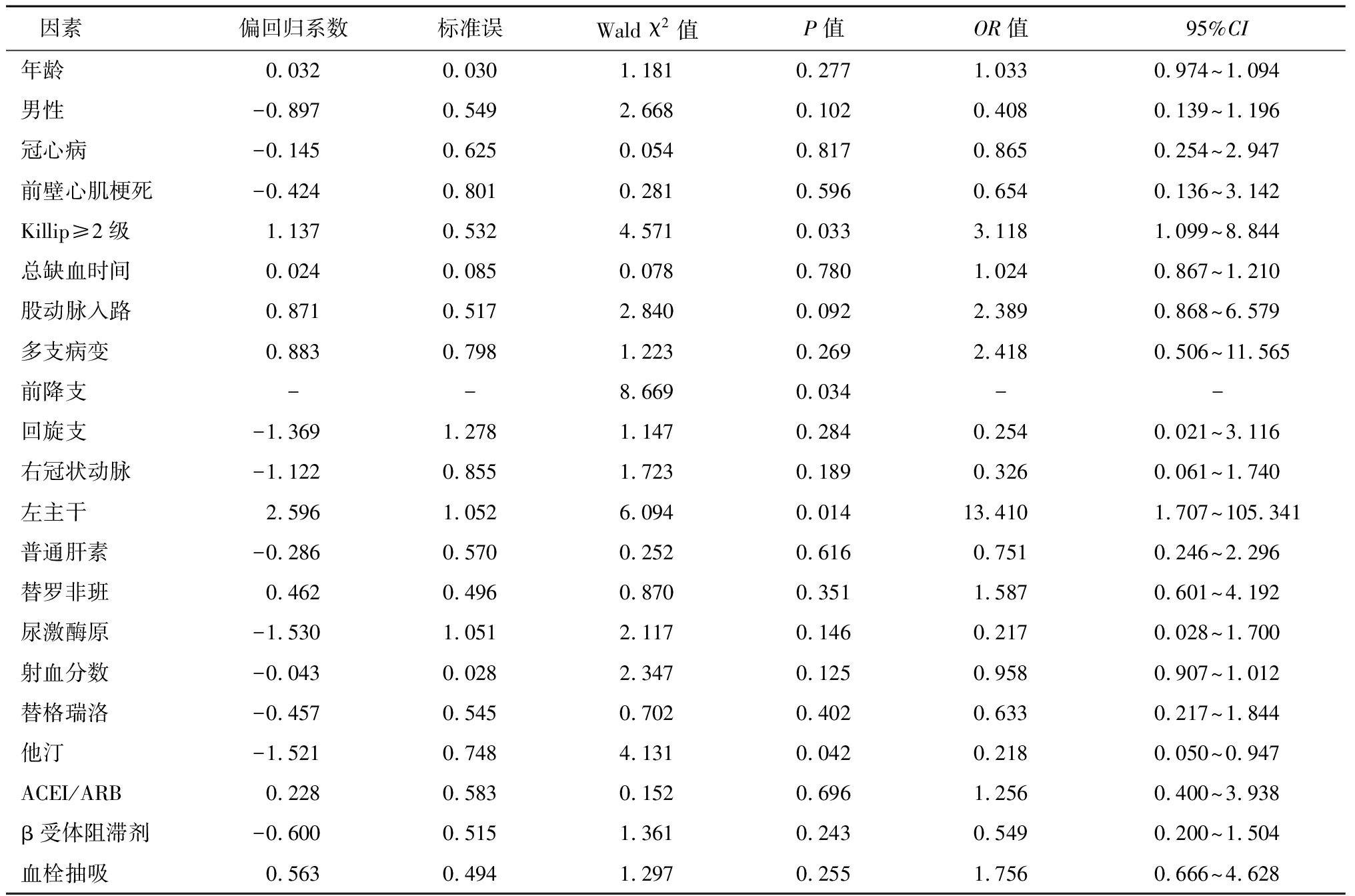
因素 偏回归系数标准误Wald χ2值P值OR值95%CI年龄0.0320.0301.1810.2771.0330.974~1.094男性-0.8970.5492.6680.1020.4080.139~1.196冠心病-0.1450.6250.0540.8170.8650.254~2.947前壁心肌梗死-0.4240.8010.2810.5960.6540.136~3.142Killip≥2级1.1370.5324.5710.0333.1181.099~8.844总缺血时间0.0240.0850.0780.7801.0240.867~1.210股动脉入路0.8710.5172.8400.0922.3890.868~6.579多支病变0.8830.7981.2230.2692.4180.506~11.565前降支--8.6690.034--回旋支-1.3691.2781.1470.2840.2540.021~3.116右冠状动脉-1.1220.8551.7230.1890.3260.061~1.740左主干2.5961.0526.0940.01413.4101.707~105.341普通肝素-0.2860.5700.2520.6160.7510.246~2.296替罗非班0.4620.4960.8700.3511.5870.601~4.192尿激酶原-1.5301.0512.1170.1460.2170.028~1.700射血分数-0.0430.0282.3470.1250.9580.907~1.012替格瑞洛-0.4570.5450.7020.4020.6330.217~1.844他汀-1.5210.7484.1310.0420.2180.050~0.947ACEI/ARB0.2280.5830.1520.6961.2560.400~3.938β受体阻滞剂-0.6000.5151.3610.2430.5490.200~1.504血栓抽吸0.5630.4941.2970.2551.7560.666~4.628
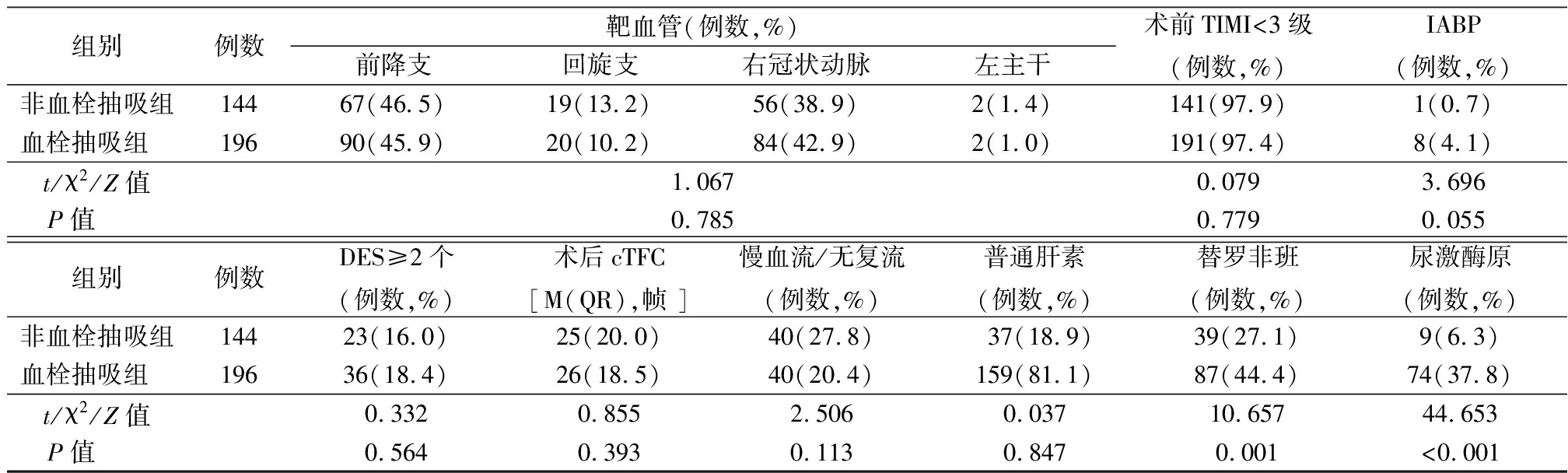
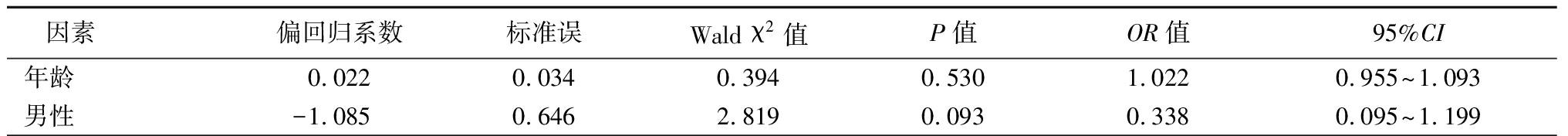
2.5 高血栓负荷亚组分析 高血栓负荷人群两组间临床基线资料比较结果同整体人群,见表5。多因素二元Logistic回归分析结果显示:血栓抽吸(OR=0.525,95%CI:0.284~0.971,P=0.04)是高血栓负荷人群术后发生无复流的保护性因素;年龄(OR=1.043,95%CI:1.013~1.074,P=0.005)、造影剂用量(OR=1.005,95%CI:1.001~1.009,P=0.018)是高血栓负荷人群发生无复流的危险因素,见表6。高血栓负荷人群两组术后12个月的MACE、心原性死亡、再发心肌梗死、靶血管重建及缺血性脑卒中发生率差异无统计学意义(P>0.05)。见表7。高血栓负荷人群两组间MACE(Log Rank=1.428,P=0.232)及心原性死亡((Log Rank=1.006,P=0.316))的Kaplan-Meier生存分析差异无统计学意义。Cox回归分析显示,血栓抽吸不是高血栓负荷人群MACE(OR=2.081,95%CI:0.617~7.014,P=0.237)及心原性死亡(OR=1.890,95%CI: 0.538~6.641,P=0.321)的影响因素,见表8。
表5 高血栓负荷人群临床基线资料比较
Table 5 Comparison of baseline, clinical and medical treatment characteristics between groups with high thrombus load
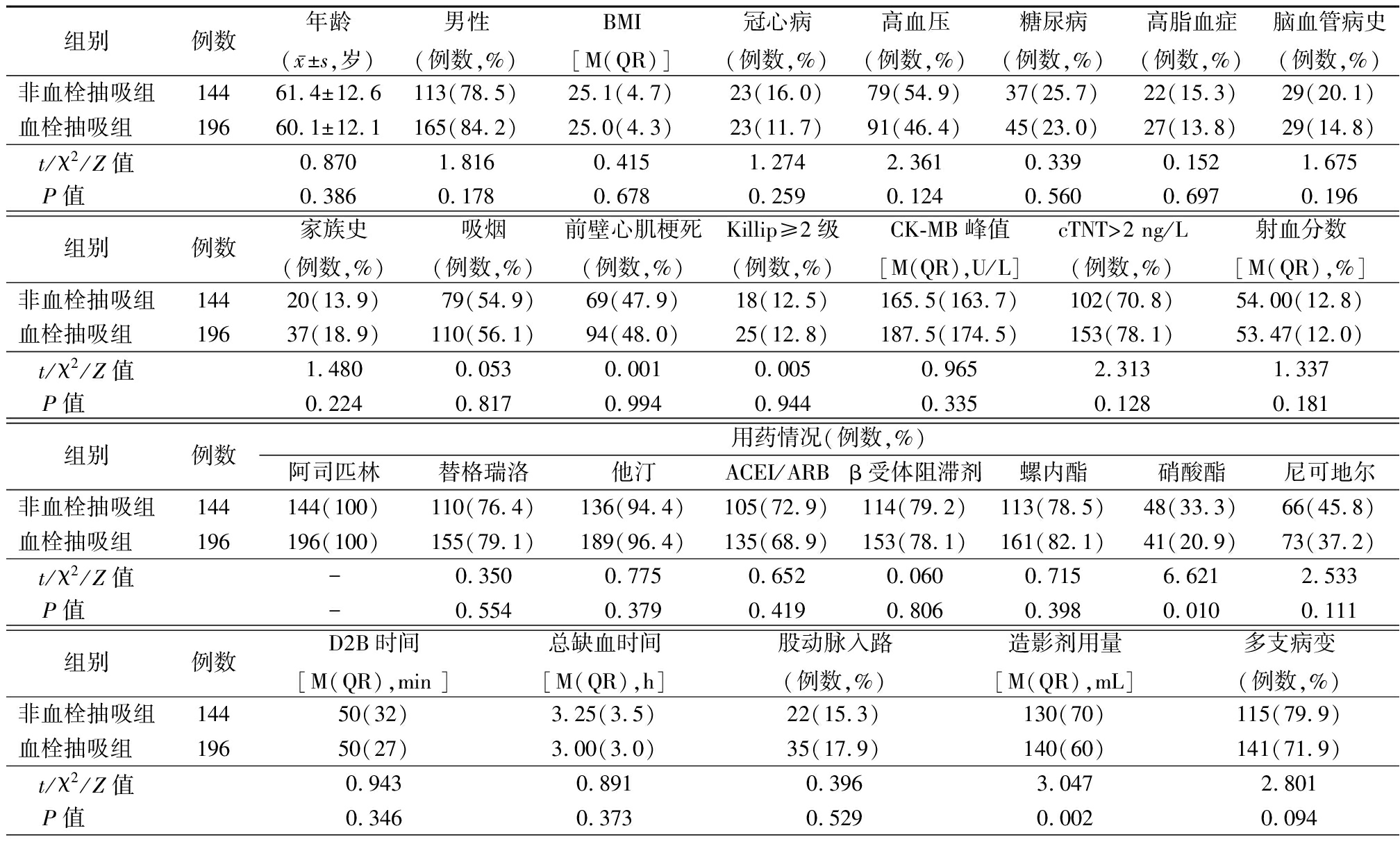
组别例数年龄(x-±s,岁)男性(例数,%)BMI[M(QR)]冠心病(例数,%)高血压(例数,%)糖尿病(例数,%)高脂血症(例数,%)脑血管病史(例数,%)非血栓抽吸组14461.4±12.6113(78.5)25.1(4.7)23(16.0)79(54.9)37(25.7)22(15.3)29(20.1)血栓抽吸组 19660.1±12.1165(84.2)25.0(4.3)23(11.7)91(46.4)45(23.0)27(13.8)29(14.8)t/χ2/Z值0.8701.8160.4151.2742.3610.3390.1521.675P值 0.3860.1780.6780.2590.1240.5600.6970.196组别例数家族史(例数,%)吸烟(例数,%)前壁心肌梗死(例数,%)Killip≥2级(例数,%)CK-MB峰值[M(QR),U/L]cTNT>2 ng/L(例数,%)射血分数[M(QR),%]非血栓抽吸组14420(13.9)79(54.9)69(47.9)18(12.5)165.5(163.7)102(70.8)54.00(12.8)血栓抽吸组 19637(18.9)110(56.1)94(48.0)25(12.8)187.5(174.5)153(78.1)53.47(12.0)t/χ2/Z值1.4800.0530.0010.0050.9652.3131.337P值 0.2240.8170.9940.9440.3350.1280.181组别例数用药情况(例数,%)阿司匹林替格瑞洛他汀ACEI/ARBβ受体阻滞剂螺内酯硝酸酯尼可地尔非血栓抽吸组144144(100)110(76.4)136(94.4)105(72.9)114(79.2)113(78.5)48(33.3)66(45.8)血栓抽吸组 196196(100)155(79.1)189(96.4)135(68.9)153(78.1)161(82.1)41(20.9)73(37.2)t/χ2/Z值-0.3500.7750.6520.0600.7156.6212.533P值 -0.5540.3790.4190.8060.3980.0100.111组别例数D2B时间[M(QR),min ]总缺血时间[M(QR),h]股动脉入路(例数,%)造影剂用量[M(QR),mL]多支病变(例数,%)非血栓抽吸组14450(32)3.25(3.5)22(15.3)130(70)115(79.9)血栓抽吸组 19650(27)3.00(3.0)35(17.9)140(60)141(71.9)t/χ2/Z值0.9430.8910.3963.0472.801P值 0.3460.3730.5290.0020.094
表5 (续)
组别例数靶血管(例数,%)前降支回旋支右冠状动脉左主干术前TIMI<3级(例数,%)IABP(例数,%)非血栓抽吸组14467(46.5)19(13.2)56(38.9)2(1.4)141(97.9)1(0.7)血栓抽吸组 19690(45.9)20(10.2)84(42.9)2(1.0)191(97.4)8(4.1)t/χ2/Z值1.0670.0793.696P值 0.7850.7790.055组别例数DES≥2个(例数,%)术后cTFC[M(QR),帧 ]慢血流/无复流(例数,%)普通肝素(例数,%)替罗非班(例数,%)尿激酶原(例数,%)非血栓抽吸组14423(16.0)25(20.0)40(27.8)37(18.9)39(27.1)9(6.3)血栓抽吸组 19636(18.4)26(18.5)40(20.4)159(81.1)87(44.4)74(37.8)t/χ2/Z值0.3320.8552.5060.03710.65744.653P值 0.5640.3930.1130.8470.001<0.001
表6 高血栓负荷人群直接冠状动脉介入治疗术后慢血流/无复流相关因素二元Logistic回归分析
Table 6 Binary Logistic regression analysis of the related factorsof slow flow/no-reflow
after PPCI in the population with high thrombus load
因素 偏回归系数标准误Wald χ2值P值OR值95%CI年龄0.0420.0158.0340.0051.0431.013~1.074男性-0.1530.3770.1640.6860.8580.410~1.798冠心病-0.2650.4150.4090.5230.7670.340~1.731高血压0.4570.2882.5140.1131.5790.898~2.775糖尿病-0.0180.3300.0030.9570.9820.514~1.877前壁心肌梗死0.0830.4320.0370.8471.0870.466~2.533Killip≥2级0.4350.3981.1910.2751.5440.708~3.371总缺血时间0.0050.0540.0090.9261.0050.904~1.118股动脉入路0.1610.3700.1890.6641.1740.569~2.425多支病变-0.4280.3511.4910.2220.6520.328~1.296前降支--2.1760.537--回旋支0.7690.5471.9750.1602.1570.738~6.303右冠状动脉0.3180.4690.4620.4971.3750.549~3.445左主干0.5341.2170.1920.6611.7050.157~18.532血栓负荷≥4级0.6951.1010.3990.5282.0040.232~17.334术前TIMI<3级0.3820.2961.6700.1961.4660.821~2.618替罗非班1.1360.8071.9800.1593.1140.640~15.155IABP-0.6440.3134.2210.0400.5250.284~0.971血栓抽吸0.3140.3580.7690.3811.3680.679~2.759尿激酶原0.2160.3980.2940.5881.2410.569~2.707普通肝素0.0050.0025.5600.0181.0051.001~1.009造影剂用量0.0420.0158.0340.0051.0431.013~1.074
表7 高血栓负荷人群直接冠状动脉介入治疗术后12个月随访的临床预后比较
Table 7 Comparison of clinical prognosis at 12-month follow-up between groups (例数,%)
组别例数MACE心原性死亡再发心肌梗死靶血管血运重建缺血性脑卒中非血栓抽吸组1345(3.7)5(3.7)2(1.5)0(0.0)2(1.5)血栓抽吸组 17512(6.9)11(6.3)3(1.7)0(0.0)6(3.4)χ2值1.4261.0090.023-1.128P值0.2320.3150.878-0.288
表8 高血栓负荷STEMI患者PPCI术后12个月发生MACE事件的多因素Cox回归分析
Table 8 Multivariate Cox regression analysis of the predictors of MACE during 12-month follow-up
after PPCI for STEMI patients with high thrombus load
因素 偏回归系数标准误Wald χ2值P值OR值95%CI年龄0.0220.0340.3940.5301.0220.955~1.093男性-1.0850.6462.8190.0930.3380.095~1.199
表8 (续)
冠心病0.2000.7070.0800.7771.2210.305~4.887前壁心肌梗死0.3541.0470.1140.7351.4250.183~11.094Killip≥2级1.3720.6115.0440.0253.9441.191~13.063总缺血时间0.0060.1010.0030.9541.0060.826~1.225股动脉入路0.7090.6311.2620.2612.0330.590~7.008多支病变0.5140.8280.3860.5341.6720.330~8.470前降支--4.3980.222--回旋支-12.964489.5980.0010.9790.0000.000右冠状动脉-0.7711.1280.4670.4940.4630.051~4.219左主干2.3651.2423.6240.05710.647 0.933~121.555普通肝素-0.4720.6760.4870.4850.6240.166~2.348替罗非班0.5810.5850.9860.3211.7880.568~5.629尿激酶原-1.2981.0731.4620.2270.2730.033~2.238射血分数-0.0730.0334.7570.0290.9300.871~0.993替格瑞洛-0.6580.6610.9910.3190.5180.142~1.891他汀-1.9410.8525.1830.0230.1440.027~0.763ACEI/ARB0.1530.7070.0470.8291.1650.292~4.653β受体阻滞剂-0.5580.6290.7860.3750.5720.167~1.965血栓抽吸0.7040.5921.4160.2342.0220.634~6.450
3 讨 论
PPCI可及时开通STEMI患者心外膜梗死相关动脉,恢复前向血流。然而,由于血栓、斑块物质移位导致的远端血管床栓塞、炎性介质及缺血导致血管内皮和心肌水肿等因素的影响,部分患者并未获得有效的心肌再灌注,影响其临床预后。血栓抽吸的原理是通过注射器抽吸产生负压,吸引出冠状动脉内血栓、斑块成分及炎症因子,减少远端微栓塞发生,降低慢血流和无复流发生,改善心肌灌注,从而改善远期预后。
REMEDIA研究首次证实PPCI术中常规血栓抽吸可提升术后心肌染色评级≥2级、心电图ST段回落≥70%患者的比率,改善心肌灌注[4]。随后的TAPAS研究也显示,PPCI中应用血栓抽吸可改善心肌组织灌注,且可降低术后1年全因死亡率、心源性死亡率以及非致命性心肌梗死发生率[5]。然而,新近发表的多项临床研究及分析显示血栓抽吸不能改善STEMI患者的心肌组织灌注和临床预后。TASTE研究显示常规血栓抽吸不能降低术后30 d、1年的全因死亡、再发心梗及支架内血栓发生率[6]。研究表明,血栓抽吸不能改善术后血流TIMI分级、心肌染色评级,未改善长期预后,且有增加术后30 d内卒中发生风险[7]。本研究显示,血栓抽吸未减少术后慢血流或无复流及临床事件发生,回归分析未显示血栓抽吸为保护因素。血栓抽吸的效果受多种因素影响,包括血栓大小、血栓成分等因素,本研究中血栓抽吸组血栓负荷≥4级,且术中应用尿激酶原、替罗非班比率均较高,提示血栓病变较重,导致未达到改善冠状动脉血流,有效改善心肌灌注,因此不能改善长期临床预后。
与Del Portillo等[8]研究相一致,血栓抽吸组患者血栓负荷≥4级比率达90.7%,远高于非血栓抽吸组,高血栓负荷是术者决定选用血栓抽吸的影响因素。研究表明高血栓负荷可增加STEMI患者死亡率,是影响STEMI患者预后的独立危险因素[9]。分析显示血栓抽吸可降低高血栓负荷患者心血管死亡风险[10]。国内学者研究显示,对于高血栓负荷的STEMI患者,血栓抽吸可提高术后冠状动脉TIMI血流3级比率,减少无复流,且可降低≤45岁高血栓负荷患者术后1年MACE发生率[11-12]。然而,也有研究表明,常规血栓抽吸可提高术后TIMI血流3级比率,但不能改善患者1年的临床预后,且有增加卒中发生风险[13]。本研究对高血栓负荷亚组分析显示,血栓抽吸是术后慢血流或无复流的保护性因素,未改善临床预后。考虑虽然冠状动脉造影示血流回复,但心肌细胞层面未达到有效再灌注,需进一步进行核素心肌灌注或心脏核磁检查。
术后脑卒中的发生率是影响PPCI术者选用血栓抽吸的重要因素。有研究表明血栓抽吸可增加卒中风险,可能由于抽吸过程中导管黏附的血栓脱落在外周,最终导致阻塞脑血管[14]。后续发表的包含25项随机对照研究,21 740例STEMI患者的荟萃分析显示,除外TOTAL研究的分析,其余并未显示血栓抽吸可增加卒中风险[15]。本研究中,血栓抽吸组的缺血性卒中发生比率高于非血栓抽吸组,差异无统计学意义,认为血栓抽吸并不增加卒中风险,其中5例患者均发生在PPCI术1个月后,此外心血管疾病患者本身为脑血管病高危人群。本研究认为高血栓负荷是影响PPCI术中应用血栓抽吸因素,血栓抽吸可降低高血栓负荷STEMI患者术后无复流和慢血流的发生率,但不能改善术后12个月的临床预后。
本研究为单中心回顾性研究,随访时间相对短,研究样本量小;未能通过核素心肌灌注显像、心脏核磁等检查准确评价心肌组织灌注;研究人群具有一定的失访率。因此有局限性,可能存在一定偏倚,临床仍需大规模随机对照研究证实。
[1] Zhang MJ,Liu X, LIU LH,et al. Correlation between intracoronary thrombus components and coronary blood flow after percutaneous coronary intervention for acute myocardial infarction at different onset time[J]. World J Clin Cases,2019,7(15):2013-2021.
[2] 中华医学会心血管病学分会,中华心血管病杂志编辑委员会.急性ST段抬高型心肌梗死诊断和治疗指南[J].中华心血管病杂志,2015,43(5):380-393.
[3] 中国医师协会心血管内科医师分会冠状动脉血栓抽吸共识专家组.冠状动脉血栓抽吸临床应用专家共识[J].中华医学杂志,2017,97(21):1624-1632.
[4] Burzotta F,Trani C,Romagnoli E,et al. Manual thrombus-aspiration improves myocardial reperfusion: the randomized evaluation of the effect of mechanical reduction of distal embolization by thrombus-aspiration in primary and rescue angioplasty(REMEDIA) trial[J]. JACC,2005,46(2):371-376.
[5] Vlaar PJ,Svilaas T,van der Horst IC,et al. Cardiac death and reinfarction after 1 year in the Thrombus Aspiration during Percutaneous coronary intervention in Acute myocardial infarction Study(TAPAS): a 1-year follow-up study[J]. Lancet,2008,371(9628):1915-1920.
[6] Lagerqvist B,Fröbert O,Olivecrona GK,et al. Outcomes 1 year after thrombus aspiration for myocardial infarction[J]. N Engl J Med,2014,371(12):1111-1120.
[7] Jolly SS,Cairns JA,Yusuf S,et al. Randomized trial of primary PCI with or without routine manual thrombectomy[J]. N Engl J Med,2015,72(15):1389-1398.
[8] Del Portillo JH,Echeverri D,Cabrales J. Association of the use of manual thrombus aspiration with intracoronary thrombotic burden in patients with ST segment elevation myocardial infarction in the real world[J]. Int J Cardiol Heart,2020,26:100436.
[9] Zhang Z,Li W,Wu W,et al. Myocardial reperfusion with tirofiban injection via aspiration catheter : Efficacy and safety in STEMI patients with large thrombus burden[J]. Herz,2020,45(3):280-287.
[10] Jolly SS,James S,Džavík V,et al. Thrombus aspiration in st-segment-elevation myocardial infarction:an individual patient meta-analysis:thrombectomytrialistscollaboration[J]. Circulation,2017,135(2):143-152.
[11] Li P,Ruan JW,Liu M,et al. Thrombus aspiration catheter improve the myocardial reperfusion of STEMI patients with high thrombus load during the emergency PCI operation[J]. J Cardiothorac Surg,2019,14(1):172.
[12] Ge J,Li J,Dong B,et al. Determinants of angiographic thrombus burden and impact of thrombus aspiration on outcome in young patients with ST-segment elevation myocardial infarction[J]. Catheter Cardiovasc Interv,2019,93(5):E269-E276.
[13] Jolly SS,Cairns JA,Lavi S,et al. Thrombus aspiration in patients with high thrombus burden in the TOTAL Trial[J]. JACC,2018,72(14):1589-1596.
[14] Keskin M,Kaya A,Tatlisu MA,et al. Effect of adjunctive thrombus aspiration on in-hospital and 3-year outcomes in patients with st-segment elevation myocardial infarction and large native coronary artery thrombus burden[J]. Am J Cardiol,2017,120(10):1708-1714.
[15] Taglieri N,BacchiReggiani ML,Ghetti G,et al. Efficacy and safety of thrombus aspiration in ST-segment elevation myocardial infarction: an updated systematic review and meta-analysis of randomised clinical trials[J]. Eur Heart J Acute Cardiovasc Care,2019,8(1):24-38.