快速康复理念是指通过各种手段优化围术期处理,减轻手术创伤疼痛,加速患者早期康复[1-2]。胃癌是常见恶性肿瘤,以外科手术治疗为主,临床上采取腹腔镜或开腹手术为常见术式。胃癌术后疼痛剧烈,且持续时间长,如果镇痛不完善可导致患者胃肠蠕动减慢、切口愈合不良、睡眠差等,术后并发症增加,因此完善镇痛有重要意义[3-4]。以往腹部手术镇痛方法主要以硬膜外镇痛或静脉镇痛为主,但两种方法各有不足[5-6]。硬膜外镇痛是腹部手术镇痛的金标准,但应用抗凝药或凝血功能异常者禁用。竖脊肌平面阻滞(erector spinae plane,ESP)是由Forero等[7]在2016年发现的一种新的阻滞技术,最先将其应用于严重胸背部神经病理性疼痛的治疗,取得良好效果。ESP阻滞感觉消失平面能达到T2~T9,并已从解剖学和影像学上证实其作用机制。国内至今鲜有ESP阻滞应用于腹部术后镇痛的公开报道,本研究拟探讨双侧竖脊肌平面阻滞复合静脉镇痛对胃癌手术患者术后早期康复的影响,并与连续硬膜外镇痛比较,为临床提供参考。
1 资料与方法
1.1 一般资料 选择2016年10月—2018年9月在我院择期行腹腔镜胃癌根治术患者60例,美国麻醉医师协会(American Society of Anesthesiologists,ASA)分级Ⅰ或Ⅱ级,采用随机数字表法将患者分为阻滞组(B组)和硬膜外组(E组),每组30例。排除标准:①严重心脑肺疾病者;②严重肝肾疾病者;③凝血功能异常者;④长期服用镇静镇痛药物、抗抑郁药物者;⑤有吸毒或酗酒史者;⑥拒绝入组或交流困难者;⑦背部穿刺点有感染者。2组性别、年龄、身高、体重、ASA分级、手术时间及术中出血量差异均无统计学意义(P>0.05),具有可比性。见表1。
表1 2组一般情况比较
Table 1 Comparison of general data between two groups ![]()
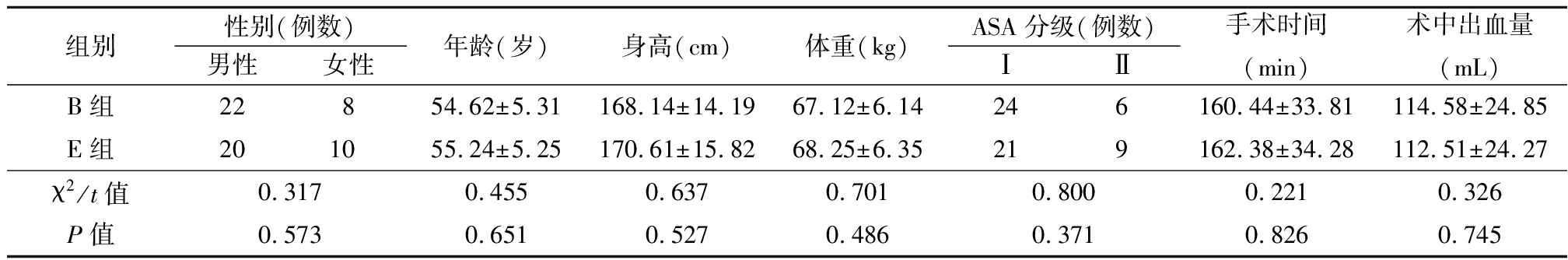
组别性别(例数)男性女性年龄(岁)身高(cm)体重(kg)ASA分级(例数)ⅠⅡ手术时间(min)术中出血量(mL)B组22854.62±5.31168.14±14.1967.12±6.14246160.44±33.81114.58±24.85E组201055.24±5.25170.61±15.8268.25±6.35219162.38±34.28112.51±24.27χ2/t值0.3170.4550.6370.7010.8000.2210.326P值0.5730.6510.5270.4860.3710.8260.745
本研究获医院医学伦理委员会批准,所有入组患者及家属均签署知情同意书。
1.2 方法 患者术前常规禁饮禁食,不使用镇静药、抗胆碱药。入室后常规行心电图、心率、血压、血氧分压和Narcotrend(NT)监测,开放上肢静脉通路,局部麻醉下行左桡动脉穿刺监测有创动脉血压。
2组均在麻醉诱导实施前行相应阻滞穿刺操作。B组行超声引导下双侧竖脊肌平面阻滞,患者取坐位,常规消毒铺巾,采用SonoSite M-turbo便携式超声仪及配套HFL38x高频探头(6~13 MHz),探头正中矢状位扫描T6棘突,探头外移3 cm至T7横突,可获得清晰竖脊肌平面图像,由浅到深分别为斜方肌、菱形肌、竖脊肌、T7横突。固定探头,采用平面外进针,清晰显示针尖,待针尖触及T7横突后回抽无血无气体后注入0.4%罗哌卡因25 mL,超声仪清晰显示药液于竖脊肌深面呈梭形扩散,注药完毕后采用相同方案行对侧竖脊肌平面阻滞。E组取侧卧位行T8~9硬膜外穿刺,穿刺成功后向头侧置入导管3 cm,回抽无血无脑脊液后注入试验剂量1.5%利多卡因3 mL,观察5 min排除导管置入血管或蛛网膜下腔后分3次注入0.4%罗哌卡因12 mL,间隔5 min。2组采用酒精棉球法测试阻滞平面,确认双侧均出现节段性阻滞后开始行麻醉诱导,所有操作均由同一名麻醉医师完成,术后由另一位不知麻药配比的麻醉医师观察并记录。两组均接受静脉全身麻醉,麻醉诱导采用舒芬太尼0.5 μg/kg、丙泊酚2 mg/kg、罗库溴铵0.5 mg/kg,气管插管后接麻醉机行机械通气。术中麻醉维持采用丙泊酚4~12 mg/kg/h、瑞芬太尼0.05~0.40 μg·kg-1·min-1、阿曲库铵0.10~0.15 mg·kg-1·h-1, NT范围维持在D2~E0。术毕2组均送至麻醉恢复室,在达到拔管标准后拔除气管导管并立即使用PCA至术后48 h,配方如下。B组:舒芬太尼2.0 μg/kg+右美托咪定1.0μg/kg+昂丹司琼8 mg+生理盐水稀释至200 mL;E组:罗哌卡因400 mg+舒芬太尼150 μg+生理盐水稀释至200 mL。2组PCA参数均设置为初始负荷剂量4 mL,维持速率4 mL/h,PCA单次剂量4 mL/次,锁定时间15 min。当静息VAS评分≥3分则按压PCA键,若效果不满意则静脉注射氟比洛芬酯50 mg,经上述处理后若仍镇痛不满意则退出本研究。
1.3 观察指标 记录术后2、4、8、12、24、48 h 的静息疼痛(visual analogue scale,VAS)(0分,无痛;10分,剧烈疼痛);记录氟比洛芬酯补救性镇痛例数、术后排气时间、首次进食时间、首次下床活动时间、住院时间和镇痛满意度评分,0~10分,分数越高,满意程度越高。记录术后48 h内镇痛相关不良反应,包括恶心呕吐、皮肤瘙痒、眩晕、呼吸抑制、尿潴留等。
1.4 统计学方法 应用SPSS 20.0统计软件分析数据。计量资料比较采用两独立样本t检验和重复测量的方差分析。计数资料比较采用χ2检验。P<0.05为差异有统计学意义。
2 结 果
2.1 2组术后不同时点静息疼痛VAS评分及补救性镇痛例数比较 2组术后静息疼痛VAS评分随术后时间越来越高,时点间差异有统计学意义(P<0.05),组间、组间·时点间交互作用差异无统计学意义(P>0.05),见表2。B组补救性镇痛例数为1例(3.3%),E组2例(6.7%),2组差异无统计学意义(χ2=0.000,P=1.000)。
表2 2组术后不同时点静息疼痛VAS评分比较
Table 2 Comparison of VAS of resting pain at different time points after operation between two groups ![]() 分)
分)
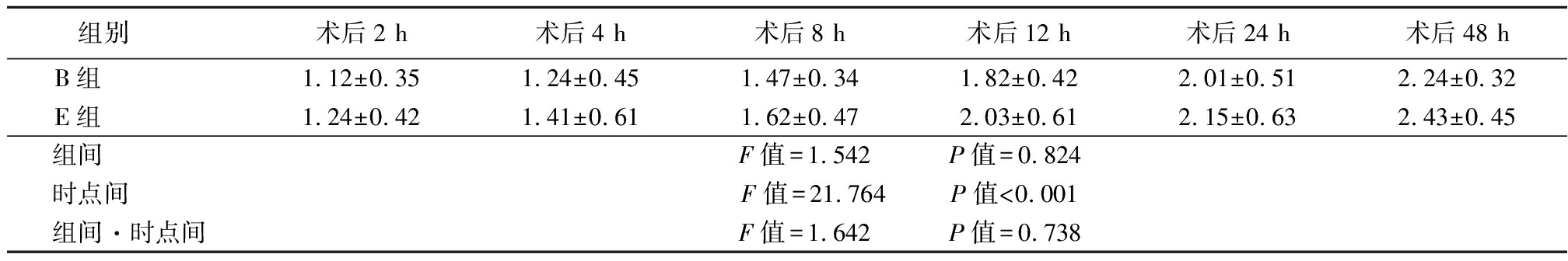
组别 术后2 h术后4 h术后8 h术后12 h术后24 h术后48 hB组 1.12±0.351.24±0.451.47±0.341.82±0.422.01±0.512.24±0.32E组 1.24±0.421.41±0.611.62±0.472.03±0.612.15±0.632.43±0.45组间 F值=1.542 P值=0.824时点间 F值=21.764 P值<0.001组间·时点间F值=1.642 P值=0.738
2.2 2组术后快速康复指标比较 B组术后排气时间、进食时间、首次下床活动时间及住院时间均明显短于E组,B组镇痛满意度明显高于E组,差异有统计学意义(P<0.05),见表3。
表3 2组术后快速康复指标比较
Table 3 Comparison of postoperative rehabilitation between two groups ![]()
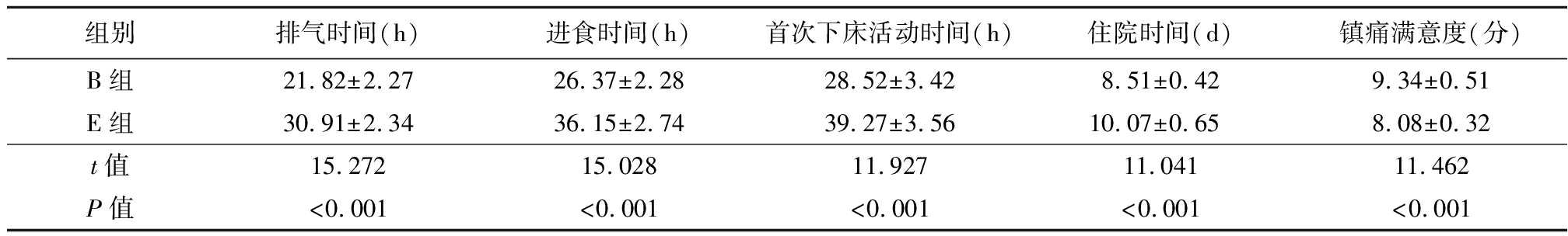
组别排气时间(h)进食时间(h)首次下床活动时间(h)住院时间(d)镇痛满意度(分)B组21.82±2.2726.37±2.2828.52±3.428.51±0.429.34±0.51E组30.91±2.3436.15±2.7439.27±3.5610.07±0.658.08±0.32t值15.27215.02811.92711.04111.462P值<0.001<0.001<0.001<0.001<0.001
2.3 2组术后48 h内镇痛相关不良反应发生情况的比较 B组术后48 h内镇痛相关不良反应发生率明显低于E组,差异有统计学意义(P<0.05),见表4。
表4 2组术后48 h内镇痛相关不良反应发生情况比较
Table 4 Comparison of postoperative adverse reactions between two groups (n=30,例数,%)
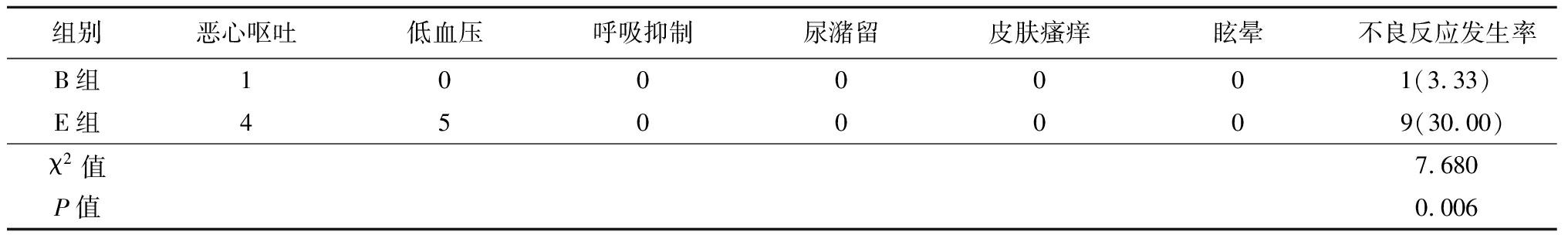
组别恶心呕吐低血压呼吸抑制尿潴留皮肤瘙痒眩晕不良反应发生率B组1000001(3.33)E组4500009(30.00)χ2值7.680P值0.006
3 讨 论
腹腔镜胃癌手术患者术后疼痛剧烈,疼痛导致机体处于持续应激状态,对神经内分泌系统、心血管系统、呼吸系统等产生不良影响,延缓患者术后快速康复[1]。完善的术后镇痛有利于患者咳嗽、咳痰及早期下床活动,降低术后肺部感染等并发症发生率。以往胃癌术后患者多采用静脉镇痛或硬膜外镇痛,但两种方法各有一定不足。静脉镇痛多采用阿片类药物,但镇痛效果一般,欲达到更好效果需加大阿片类药物使用剂量,但眩晕、尿潴留、恶心呕吐、皮肤瘙痒、呼吸抑制等不良反应发生率明显增加,硬膜外镇痛是胸腹部术后镇痛的金标准,虽然镇痛效果完善,但对患者生理功能干扰大,容易出现低血压或尿潴留,且中位硬膜外穿刺操作难度大,若患者存在凝血异常或长期应用抗凝药物,硬膜外镇痛则为禁忌[8]。
近年来随着可视化技术发展,超声引导腹壁神经阻滞被广泛应用于腹部术后镇痛。这类阻滞技术能有效缓解患者腹部术后疼痛,减轻应激反应,减少呼吸循环系统并发症发生,同时减少术后阿片类药物的应用,减轻单用阿片类药物引起的恶心呕吐、皮肤瘙痒等不良反应,促进患者早期下床活动,加速患者术后快速康复。但由于这类阻滞技术仅能有效解决腹部术后切口疼痛,对内脏痛效果差,因此临床上一直在寻找更安全有效的辅助镇痛方法[9]。
ESP阻滞产生多节段阻滞作用的机制可能与以下几方面相关:①由于竖脊肌覆盖整个背部,ESP阻滞后局部麻醉可往头尾方向广泛扩散至多个神经支配区;②注药位置在横突上,与椎旁间隙或椎间孔位置邻近,局麻药可扩散至椎旁间隙或经椎间孔进入硬膜外腔[10]。本研究中,阻滞组采用双侧竖脊肌平面阻滞联合静脉镇痛,硬膜外组采用连续硬膜外镇痛,术后各时点2组静息疼痛VAS评分比较无明显差异且均低于3分,说明两种镇痛方法均能为腹腔镜胃癌手术患者提供较长时间的完善术后镇痛。腹部术后疼痛机制非常复杂,疼痛一方面来源于腹壁切口创伤,另外一方面与腹腔内脏创伤或牵拉有关。手术创伤可以直接导致组织水肿、炎症反应等导致疼痛发生,局部疼痛通过复杂的传导机制导致疼痛外周和中枢敏化。神经阻滞或椎管内麻醉均可有效预防疼痛外周和中枢敏化,起到良好缓解疼痛作用[11]。
快速康复理念是指通过各种手段优化围术期处理,减轻手术创伤疼痛,加速患者早期康复[1,12]。良好的术后镇痛可促使患者胃肠道功能早期恢复,及早下床活动,加速患者早期康复。本研究选择术后静息疼痛VAS评分、术后排气时间、首次进食时间、首次下床活动时间、镇痛期间不良反应发生情况等指标综合评估患者快速康复情况,显示阻滞组上述指标明显低于硬膜外组,提示双侧竖脊肌平面阻滞联合静脉镇痛相对连续硬膜外镇痛更能促进胃癌患者术后早期康复。阻滞组优于硬膜外组原因可能是:①硬膜外镇痛可同时阻滞交感神经和运动神经,假如阻滞平面过于宽广,可能引起部分肋间肌或心交感神经被阻滞,影响患者呼吸功能恢复或发生低血压、心动过缓等;②硬膜外导管随着患者体位改变发生卡压或导管脱落,导致镇痛中断;③采用连续硬膜外镇痛由于担心导管脱落等原因导致行动不便限制患者早期下床活动。早期下床活动是影响住院时间的重要因素之一,采用神经阻滞联合静脉多模式镇痛能减轻患者心理负担,使患者尽早下床活动,并促进胃肠道蠕动,患者早期康复加速,同时静脉镇痛自控性好、患者依从性及满意度较高[13-15]。
综上所述,双侧竖脊肌平面阻滞复合静脉镇痛与连续硬膜外镇痛均能为胃癌手术患者提供良好术后镇痛,但前者不良反应更少,患者满意度更高,更有利于患者早期快速康复,缩短住院时间。
[1] 黄永侨,华福洲,邬林泉,等.加速康复外科理念下不同镇痛方式对肝切除术后早期康复的影响[J].临床麻醉学杂志,2017,33(2):140-143.
[2] 陈延云,于玲,谭宏宇.羟考酮联合右美托咪啶对腹腔镜胃癌患者术后的镇痛效果[J].实用医学杂志,2017,33(22):3795-3798.
[3] Brackstone M. A review of the literature and discussion:establishing a consensus for the definition of post-mastectomy pain syndrome to provide a standardized clinical and research approach[J]. Can J Surg,2016,59(5):294-295.
[4] Elamin G,Waters PS,Hamid H,et al. Efficacy of a Laparoscopically delivered transversus abdominis plane block technique during elective laparoscopic cholecystectomy:a prospective,double-blind randomized Trial[J].J Am Coll Surg,2015,221(2):335-344.
[5] Dizdarevic A,Fernandes A. Thoracic paravertebral block,multimodal analgesia,and monitored anesthesia care for breast cancer surgery in primary lateral sclerosis[J]. Case Rep Anesthesiol, 2016,2016:6301358.
[6] Tam KW,Chen SY,Huang TW,et al. Effect of wound infiltration with ropivacaine or bupivacai-ne analgesia in breast cancer surgery:a meta-analysis of randomized controlledtrials[J]. Int J Surg, 2015, 22:79-85.
[7] Forero M,Adhikary SD,Lopez H,et al. The erector spinae plane block:anovel analgesic technique in thoracic neuropathic pain[J]. Reg Anesth Pain Med,2016,41(5):621-627.
[8] 张俊杰,李曼,曹亚楠,等.罗哌卡因双侧胸椎旁神经阻滞对心肺转流心脏瓣膜手术后康复的影响[J].临床麻醉学杂志,2017,33(12):1178-1180.
[9] 刘建军,袁西景,阚和平.有效镇痛对肝癌术后肝功能恢复的影响[J].实用医学杂志,2017,33(15):2517-2520.
[10] 马丹旭,任惠龙,芮燕,等.超声引导下单次竖脊肌平面阻滞对胸腔镜下肺叶切除患者静脉自控镇痛效果的影响[J].临床麻醉学杂志,2017,33(10):965-967.
[11] Kaufman E,Epstein JB,Gorsky M,et al. Preemptive analgesia and local anesthesia as a supplement to general anesthesia: a review[J]. Anesth Prog,2005,52(1):29-38.
[12] Dorcaratto D,Grande L,Pera M. Enhanced recovery in gastrointestinal surgery:upper gastrointestinal surgery[J]. Dig Surg,2013,30(1):70-78.
[13] Marjanski T,Wnuk D,Bosakowski D,et al. Patients who do not reach a distance of 500 mduring the 6-min walk test have an increased risk of postoperative complications and prolonged hospital stay after lobectomy[J]. Eur J Cardiothorac Surg,2015,47(5):e213-e219.
[14] 董秋月,陈双涛,孟华.收肌管阻滞与股神经阻滞用于全膝关节置换术后镇痛效果比较[J].河北医科大学学报,2018,39(10):1213-1217.
[15] 张隆盛,林旭林,张欢楷.超声引导腰方肌阻滞对剖宫产术后镇痛的影响[J].河北医科大学学报,2018,39(9):1053-1057.