卵巢癌是一种致命的妇科恶性肿瘤[1],也是全球妇科恶性肿瘤中存活率最低的疾病[2]。因其前期症状不明显,晚期表现出症状时常伴有广泛的转移,多数患者确诊时已发展至晚期[3]。在初步诊断时,超过四分之三的卵巢癌患者处于Ⅲ~Ⅳ期,5年生存率低于30%[4],患者生活质量受到严重影响。在正常女性阴道中乳杆菌是阴道内的优势菌,其对维持阴道微环境起着重要作用,在避免生殖道感染方面起着至关重要的作用[5]。研究表明,乳杆菌可以通过维持pH值和产生物种代谢物来抵御病原体感染[6]。妇科生殖健康疾病在世界范围内常见,在整个生命过程中对女性的身心健康产生重要影响。然而卵巢癌患者可因免疫力降低、内分泌功能变化、激素改变等因素影响,发生阴道感染性疾病,对患者预后及生活质量产生不良影响。同时值得注意的是阴道炎可能也对患者疾病产生不良影响,长期阴道炎会导致妇科肿瘤癌前病变的风险增加[7]。国内外对育龄期及宫颈癌患者阴道微生态及危险因素分析较多,对卵巢癌患者群体报道较少。本研究对卵巢癌合并阴道炎患者阴道微生态特征及危险因素进行分析,为临床预防及治疗提供参考。
1 资 料 与 方 法
1.1 一般资料 选取2019年河南省焦作市第五人民医院、河南省焦作市妇幼保健院、江苏省盐城市第六人民医院、上海同济大学附属同济医院收治的卵巢癌患者330例,年龄33~67岁。纳入标准:①切除术前行分泌物采集;②7 d以上无性生活;③近7 d无阴道冲洗。排除标准:①妊娠期;②使用激素或免疫抑制剂;③合并其他妇科肿瘤及其他部位肿瘤;④资料不齐全。
1.2 标本收集及检测 专业医生使用无菌棉签从阴道侧壁上1/3处收集分泌物2只送检,1只分泌物涂片、干燥、固定后革兰染色,油镜下观察菌群、滴虫、病原菌等指标;1只分泌物行阴道炎五项联检试剂检测。
1.3 诊断标准 阴道炎诊断标准依据2016年中华医学会妇产科学会发布的专家共识[8],①正常阴道微生态:菌群密集度(Ⅱ~Ⅲ级)、多样性(Ⅱ~Ⅲ级)、乳杆菌为主、pH值3.8~4.5、白细胞酯酶等阴性,其中1项异常即微生态失调;②滴虫性阴道炎(trichomonal vaginitis,TV):找到滴虫;③细菌性阴道炎(bacterial vaginosis,BV):Nugent评分≥7分;④阴道假丝酵母菌病(vulvovaginal candidiasis,VVC):找到假菌丝或芽生孢子;⑤混合感染:两种及以上混合阴道炎感染;⑥需氧性阴道炎(aerobic vaginitis,AV):Donders评分≥3分;⑦革兰染色形态学与阴道炎五项联检检测结果不一致时,以形态学检验为依据。
1.4 危险因素分析 回顾性分析330例卵巢癌患者的临床资料,包括年龄、文化程度、基础疾病、避孕套使用、性生活频率、化疗、自行阴道冲洗、阴道炎史。
1.5 统计学方法 应用SPSS 25.0统计软件分析数据。计数资料比较采用χ2检验,影响因素确定采用多因素Logistic回归分析,采用Graphpad 8.0绘制多因素回归分析森林图,ROC曲线评价Logistic回归分析模型。P<0.05为差异有统计学意义。
2 结 果
2.1 卵巢癌合并阴道炎患者感染特征及其构成比 330例卵巢癌患者中合并阴道炎感染患者117例(35.45%)。117例合并阴道炎感染患者中感染类型构成比由多到少依次为:VVC 35例(29.91%),BV 30例(25.64%),微生态失调28例(23.93%),混合感染14例(11.97%),AV 8例(6.84%),TV 2例(1.71%)。
2.2 卵巢癌合并阴道炎患者感染的单因素分析 感染组年龄≥50岁、有基础疾病、性生活频率≥2次/周、化疗、自行阴道冲洗、阴道炎史比例高于非感染组,专科及以上文化程度、使用避孕套比例低于非感染组,差异有统计学意义(P<0.05),见表1。
表1 卵巢癌合并阴道炎患者感染的单因素分析
Table 1 Univariate analysis of infection in patients with ovarian cancer complicated with vaginitis (例数,%)
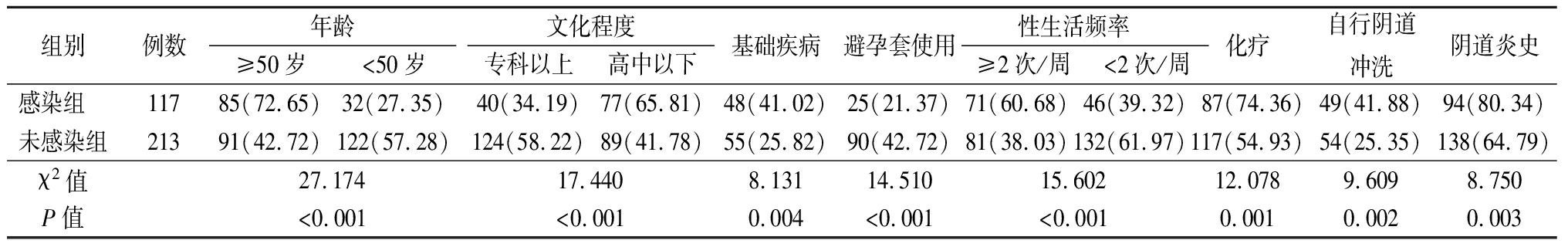
组别例数年龄 ≥50岁<50岁文化程度专科以上高中以下基础疾病避孕套使用性生活频率≥2次/周<2次/周化疗自行阴道冲洗阴道炎史感染组 11785(72.65)32(27.35)40(34.19)77(65.81)48(41.02)25(21.37)71(60.68)46(39.32)87(74.36)49(41.88)94(80.34)未感染组21391(42.72)122(57.28)124(58.22)89(41.78)55(25.82)90(42.72)81(38.03)132(61.97)117(54.93)54(25.35)138(64.79)χ2值27.17417.4408.13114.51015.60212.0789.6098.750P值<0.001<0.0010.004<0.001<0.0010.0010.0020.003
2.3 卵巢癌合并阴道炎患者感染多因素回归分析 以卵巢癌合并阴道炎(是=1,否=0)为因变量,以年龄(≥50岁=1,<50岁=0)、文化程度(专科以上=1,高中以下=0)、使用避孕套(是=1,否=0)、基础疾病(是=1,否=0)、化疗(是=1,否=0)、性生活频率(≥2次/周=1,<2次/周=0)、自行阴道冲洗(是=1,否=0)、阴道炎史(是=1,否=0)为自变量进行多因素Logistic回归分析,结果显示,年龄≥50岁、基础疾病、性生活频率≥2次/周、化疗、自行阴道冲洗、阴道炎史是卵巢癌合并阴道炎感染的危险因素,文化程度专科以上、使用避孕套是卵巢癌合并阴道炎感染的保护因素(P<0.05),见表2。多因素Logistic回归分析森林图见图1。

图1 卵巢癌合并阴道炎患者感染多因素Logistic回归分析森林图
Figure 1 Multivariate Logistic regression analysis of forest plot of infection in patients with ovarian cancer complicated with vaginitis
表2 卵巢癌合并阴道炎患者感染多因素Logistic回归分析
Table 2 Multivariate Logistic regression analysis of infection in patients with ovarian cancer complicated with vaginitis
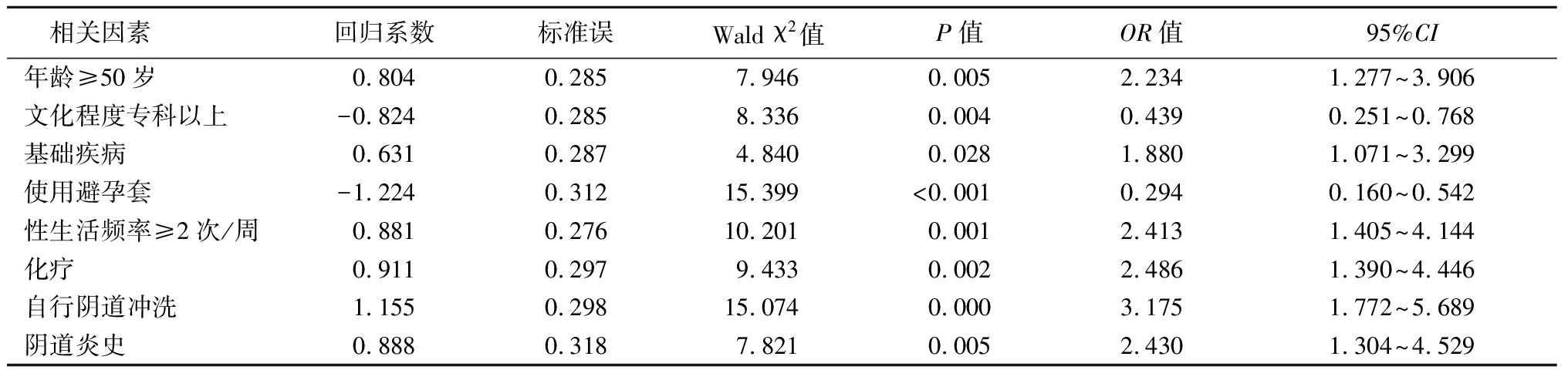
相关因素回归系数标准误Wald χ2 值P值OR值95%CI年龄≥50岁0.8040.2857.9460.0052.2341.277~3.906文化程度专科以上-0.8240.2858.3360.0040.4390.251~0.768基础疾病0.6310.2874.8400.0281.8801.071~3.299使用避孕套-1.2240.31215.399<0.0010.2940.160~0.542性生活频率≥2次/周0.8810.27610.2010.0012.4131.405~4.144化疗0.9110.2979.4330.0022.4861.390~4.446自行阴道冲洗1.1550.29815.0740.0003.1751.772~5.689阴道炎史0.8880.3187.8210.0052.4301.304~4.529
2.4 ROC曲线评价Logistic回归分析模型 应用ROC曲线对Logistic回归模型预测因子进行模型结果分析,结果显示,曲线下面积为0.808,95%CI:0.762~0.849)。与机会线下面积比较差异有统计学意义(Z=12.448,P<0.001)。提示预测模型结果较好,可较好反映卵巢癌合并阴道炎患者感染的影响因素,见图2。
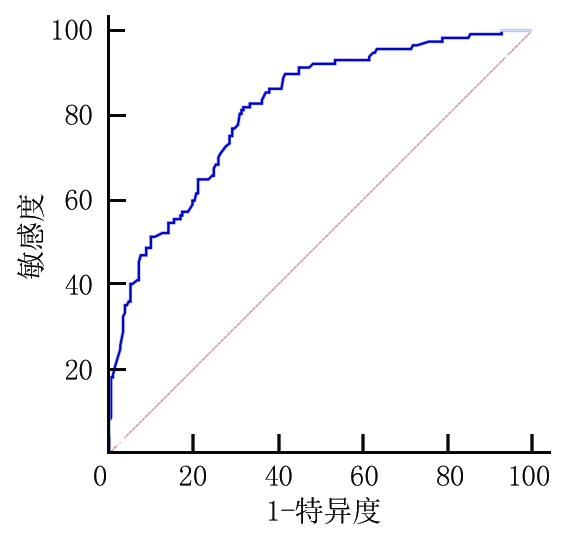
图2 多因素Logistic回归预测模型分析ROC曲线图
Figure 2 ROC curve of multivariate Logistic regression prediction model analysis
3 讨 论
因卵巢癌在早期检测阶段没有特定的生物标志物,成为女性死亡风险最高的癌症之一[9]。由于卵巢癌的高患病率和不断上升的发病率,其对个人健康和生活质量构成了重大威胁[10]。卵巢癌患者因抵抗力低下,在长时间受病痛困扰的同时如果合并阴道炎感染,则会对患者身心及生活质量造成严重影响,因此对其阴道感染特征及危险因素进行分析有着重要的意义。
本研究结果显示,330例卵巢癌中合并阴道炎感染患者117例(35.45%)。117例合并阴道炎感染患者中感染类型前三位依次为VVC 35例(29.91%)、BV 30例(25.64%)、微生态失调28例(23.93%)。感染检出率低于李金凤[11]报道成年女性人群检出率近10%,感染类型构成与其结果基本相近,只是构成比方面略有差异,可能与研究人群不同有关。VVC、BV是常见的生殖道疾病,每年影响数百万女性,超过四分之三的妇女一生中至少会感染一次VVC,其中近半数的患者会出现二次复发[12],BV感染占阴道感染的三分之一[13]。生理变化、免疫力下降、激素水平升高等都与VVC及BV感染风险相关[14]。全球范围内生殖道感染疾病对人类身体、情感和经济负担产生了巨大影响[15]。因此提示临床需对卵巢癌患者生殖卫生健康引起关注,特别是VVC、BV、微生态失调等引起的阴道感染,加强此类疾病方面的监测。经多因素Logistic回归分析,结果显示,年龄≥50岁、基础疾病、自行阴道冲洗、性生活频率≥2次/周、化疗、阴道炎史是卵巢癌合并阴道炎感染的危险因素,提示多种因素可致卵巢癌患者合并阴道炎的感染。年龄增加可致机体机能减弱,身体抵抗力下降,对病原菌的易感性增加[16]。阴道由于生理位置特殊,病症易出现迁延不愈状况,更增加了卵巢癌患者合并感染的风险。同时年龄≥50岁患者处于绝经期前后,体内激素水平较低致阴道上皮细胞糖原分泌减少,pH值增高抑制乳杆菌生长,更利于病原菌的滋生[17]。因此应对年龄≥50岁卵巢癌患者阴道菌群进行监测,防止阴道炎的发生。基础疾病可因多种因素致患者免疫力降低,加重感染的风险。卵巢癌患者术前化疗在减灭肿瘤细胞同时,会对机体免疫防御系统产生损害及组织器官的损伤,使得菌群种类、数量发生变化,增加了阴道微生态失调概率[18]。当化疗次数增多,机体免疫力和骨髓造血能力受到抑制,导致抗菌卫士白细胞及中性粒细胞不足,同样增加了阴道感染的发生[19]。化疗患者应注重提高患者机体免疫力,关注阴道微生态变化,适当时可给予免疫增强剂。有阴道炎史患者是无阴道炎史患者发生合并感染的2.43倍,可能与阴道炎不规范治疗易复发、局部pH值及微生态菌群发生变化有关。性生活频率≥2次/周发生感染风险增加2.413倍,频繁的性生活阻碍了后期阴道生态系统的恢复,为病原菌的生长提供了理想的环境,同时频繁的性生活会增加肛周和外阴周围细菌转移到阴道的可能性,从而导致感染发生[20]。频繁自行阴道冲洗可致阴道黏膜损伤、防御功能受损及不规范操作将外源性细菌带入阴道,且阴道洗液同时可抑制乳杆菌致使微生态改变[21]。因此对于有自行阴道冲洗及性生活频繁的患者,应加强生殖卫生保健方面的知识普及。文化程度专科以上、使用避孕套是卵巢癌合并阴道炎感染的保护因素,文化程度高的患者接受的教育及生理健康预防知识相对较多,也更加注重个人健康以及重视就诊治疗,因此文化程度较低患者应重视其生理健康科普知识认知。安全套使用可避免男性外阴病原菌带入阴道,因此应鼓励性生活时使用安全套,降低合并感染阴道炎的风险。
综上所述,卵巢癌合并阴道炎患者以VVC为主,BV次之。年龄、基础疾病、性生活频率、化疗、自行阴道冲洗、阴道炎史是卵巢癌合并阴道炎感染的危险因素,文化程度专科以上及使用避孕套是卵巢癌合并阴道炎感染的保护因素。临床应依据感染特征及危险因素,制定针对性的措施进行干预。纠正危险因素涉及的不良生活习惯,加强生理健康知识及疾病预防知识的普及。
[1] Bacalbasa N,Balescu I,Dima S,et al. Extended pelvic resections as part of secondary cytoreduction for relapsed ovarian adenocarcinoma[J]. In Vivo,2020,34(1):397-400.
[2] Liu C,Bordeaux A,Hettich S,et al. MicroRNA-497-5p functions as a modulator of apoptosis by regulating metadherin in ovarian cancer[J]. Cell Transplant,2020,29:963689719897061.
[3] Manai M,Doghri R,Finetti P,et al. Overexpression of annexin A1 is an independent predictor of longer overall survival in epithelial ovarian cancer[J]. In Vivo,2020,34(1):177-184.
[4] Feng LY,Liao SB,Li L. Preoperative serum levels of HE4 and CA125 predict primary optimal cytoreduction in advanced epithelial ovarian cancer:a preliminary model study[J]. J Ovarian Res,2020,13(1):17.
[5] Kovachev S. Defence factors of vaginal lactobacilli[J]. Crit Rev Microbiol,2018,44(1):31-39.
[6] Li L,Ding L,Gao T,et al. Association between vaginal micro-environment disorder and cervical intraepithelial neoplasia in a community based population in China[J]. J Cancer,2020,11(2):284-291.
[7] Muls A,Andreyev J,Lalondrelle S,et al. Systematic review:the impact of cancer treatment on the gut and vaginal microbiome in women with a gynecological malignancy[J]. Int J Gynecol Cancer,2017,27(7):1550-1559.
[8] 中华医学会妇产科学分会感染性疾病协作组.阴道微生态评价的临床应用专家共识[J].中华妇产科杂志,2016,51(10):721-723.
[9] Vellingiri B,Iyer M,Devi Subramaniam M,et al. Understanding the role of the transcription factor Sp1 in ovarian cancer:from theory to practice[J]. Int J Mol Sci,2020,21(3):1153.
[10] Mahalaxmi I,Devi SM,Kaavya J,et al. New insight into NANOG:a novel therapeutic target for ovarian cancer(OC)[J]. Eur J Pharmacol,2019,852:51-57.
[11] 李金凤.2178例女性阴道分泌物检测结果的临床分析[J].国际检验医学杂志,2017,38(14):1993-1995.
[12] Djohan V,Angora KE,Vanga-Bosson AH,et al. Recurrent vulvo-vaginal candidiasis in abidjan(Cǒte d′Ivoire):aetiology and associated factors[J]. J Mycol Med,2019,29(2):127-131.
[13] Kamga YM,Ngunde JP,Akoachere J. Prevalence of bacterial vaginosis and associated risk factors in pregnant women receiving antenatal care at the kumba health district(KHD),cameroon[J]. BMC Pregnancy Childbirth,2019,19(1):166.
[14] Zeng X,Zhang Y,Zhang T,et al. Risk factors of vulvovaginal candidiasis among women of reproductive age in Xi′an:a cross-sectional study[J]. Biomed Res Int,2018,2018:9703754.
[15] Collins LM,Moore R,Sobel JD. Prognosis and long-term outcome of women with idiopathic recurrent vulvovaginal candidiasis caused by candida albicans[J]. J Low Genit Tract Dis,2020,24(1):48-52.
[16] 王美藏,高建宏,杨雅琴,等.HPV感染患者阴道菌群与宫颈局部免疫功能的相关性研究[J].河北医科大学学报,2018,39(1):104-107.
[17] 陈婉珍,闫颖,吴林玲.妊娠期妇女阴道微生态研究进展[J].中国微生态学杂志,2016,28(4):489-492,497.
[18] 张晗,林琳,杞朝梅,等.宫颈癌患者阴道微生态研究进展[J].中国妇幼卫生杂志,2019,10(5):91-94.
[19] Leary A,Cowan R,Chi D,et al. Primary surgery or neoadjuvant chemotherapy in advanced ovarian cancer:the debate continues[J]. Am Soc Clin Oncol Educ Book,2016,35:153-162.
[20] Abdul-Aziz M,Mahdy M,Abdul-Ghani R,et al. Bacterial vaginosis,vulvovaginal candidiasis and trichomonal vaginitis among reproductive-aged women seeking primary healthcare in Sana′a city,Yemen[J]. BMC Infect Dis,2019,19(1):879.
[21] Abdullateef RM,Ijaiya MA,Abayomi F,et al. Bacterial vaginosis:prevalence and associated risk factors among non-pregnant women of reproductive age attending a nigerian tertiary hospital[J]. Malawi Med J,2017,29(4):290-293.