经皮椎体后凸成形术(percutaneous kyphoplasty,PKP)是治疗老年骨质疏松性胸腰椎压缩性骨折的常用术式,具有创伤小、显著缓解疼痛、提高患者生存率及生活质量的优点[1-2]。PKP一般在局部麻醉下进行,然而局部麻醉难以控制术中骨穿刺、球囊扩张以及骨水泥注入时产生的疼痛及紧张、焦虑等不良反应,导致镇痛效果不理想,患者体验差,同时,疼痛继发的血流动力学异常,导致心脑血管意外事件出现风险明显增大[3]。有研究报道,在全身麻醉下施行PKP,虽然镇痛效果显著,但需气管插管,操作复杂、费用高,对高龄患者麻醉风险高、并发症发生率高,并未在临床广泛开展[4]。目前,有少量文献报道,静脉麻醉下的PKP手术取得了一定的效果[5-7],但缺乏专门针对高龄患者(年龄≥80岁)实施静脉麻醉的相关研究。本研究回顾性分析了我科应用右美托咪定静脉麻醉联合局部麻醉下行PKP手术的高龄患者的临床资料,旨在探讨静脉麻醉联合局部麻醉用于高龄患者PKP的效果。报告如下。
1 资料与方法
1.1 一般资料 选择2019年7月—2020年7月于我科行PKP的高龄(年龄≥80岁)胸腰椎骨折患者36例,所有患者术前经病史采集、临床检查评价神经功能、脊柱正侧位X线片、CT及MRI影像确诊为单椎体骨折。根据美国麻醉医师协会(American Society of Anesthesiologists,ASA)评分评价患者麻醉相关风险。根据是否联合静脉麻醉分为静脉麻醉联合局部麻醉组(观察组)19例和局部麻醉组(对照组)17例,2组性别、年龄、体重、ASA分级差异无统计学意义(P>0.05),具有可比性。见表1。
表1 2组一般情况比较
Table 1 Comparison of general conditions between two groups
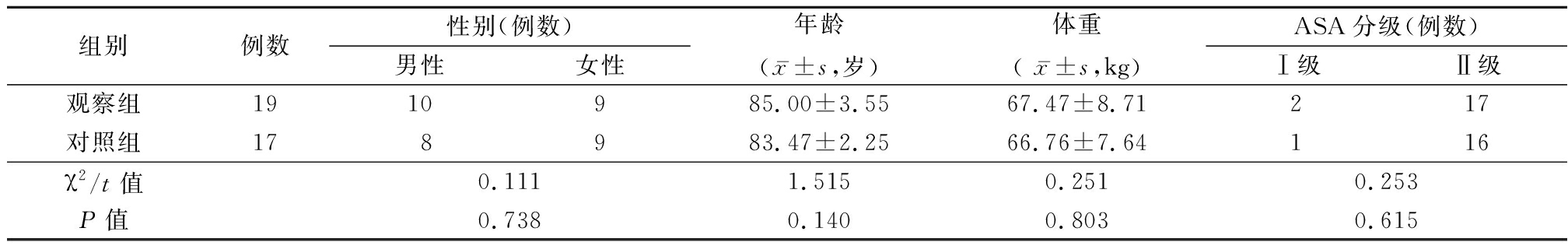
组别例数性别(例数)男性女性年龄(x-±s,岁)体重( x-±s,kg)ASA分级(例数)Ⅰ级Ⅱ级观察组1910985.00±3.5567.47±8.71217对照组178983.47±2.2566.76±7.64116χ2/t值0.1111.5150.2510.253P值0.7380.1400.8030.615
1.2 纳入标准和排除标准 纳入标准:①年龄≥80岁,经临床、影像学诊断为骨质疏松性压缩性胸腰椎骨折(Magerl[8] A 型),并且疼痛症状持续不能缓解或为防止长期卧床引发的并发症,需要手术干预者;② ASA分级为Ⅰ级或Ⅱ级,术前心、肺、肝、肾、凝血功能等未见明显异常;③血压、血糖控制稳定,停用抗血小板药物5~7 d,采用PKP手术治疗。排除标准:①结核、肿瘤等其他原因引起的非骨质疏松性脊柱骨折者;②伴有意识障碍或精神、神经病史者;③长期服用镇静、镇痛药物者;④合并有房室传导阻滞、窦性心动过缓、窦房结综合征者;⑤存在明显手术禁忌证或采用非手术治疗者。
1.3 方法 2组患者予以常规术前准备,入手术室后常规鼻导管吸氧,氧流量2 L/min,监测心电图、平均动脉压(mean arterial pressure,MAP)、心率(heart rate,HR)、血氧饱和度(blood oxygen saturation,SpO2),建立静脉通道。所有患者的麻醉监护由同一组麻醉师实施,手术由同一组外科医师完成。采用1.0%利多卡因40 mL行皮肤至伤椎骨膜的逐层浸润麻醉,按照规程经双侧椎弓根入路行PKP。观察组术前10 min经静脉滴注右美托咪定,给药浓度4 mg/L,以0.5 μg/kg为负荷剂量持续泵入,后以0.4 μg·kg-1·h-1维持至手术结束。术中镇静深度根据患者疼痛反应,如动作或面部表情及生命体征变化等判断,药物的用量参考上诉指标予以调整。
1.4 观测指标 ①观察并记录2组患者手术时间(min)。②术后第1天采用“5分制”评价围手术期疼痛管理的满意度评分,1分,非常不满意;2分,不满意;3分,一般;4分,满意;5分,非常满意。③记录术前(T0)、局部麻醉时(T1)、穿刺入椎体时(T2)、球囊扩张时(T3)、注入骨水泥时(T4)、手术结束时(T5)的MAP、HR、SpO2和腰痛VAS评分。④记录2组围手术期麻醉不良反应及并发症发生情况。
1.5 统计学方法 应用SPSS 20.0统计学软件分析数据。计量资料比较采用独立样本t检验和重复测量的方差分析,计数资料比较采用χ2检验。P<0.05为差异有统计学意义。
2 结 果
2.1 2组手术时间及满意度评分比较 2组手术时间差异无统计学意义(P>0.05);观察组围手术期疼痛管理满意度评高于对照组,差异有统计学意义(P<0.05)。见表2。
表2 2组手术时间和满意度评分比较
Table 2 Comparison of duration of operation and
satisfaction scores between two groups![]()
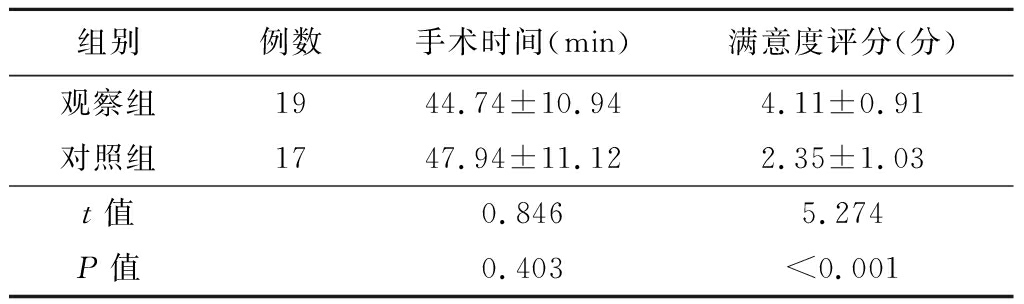
组别例数手术时间(min)满意度评分(分)观察组1944.74±10.944.11±0.91对照组1747.94±11.122.35±1.03t值0.8465.274P值0.403<0.001
2.2 2组MAP、HR、SpO2、VAS评分比较 2组患者MAP、HR、VAS评分变化趋势波动,观察组患者MAP、HR、VAS评分低于对照组,组间、时点间、组间·时点间交互作用差异有统计学意义(P<0.05);2组SpO2时点间差异有统计学意义(P<0.05),组间、组间·时点间交互作用差异无统计学意义(P>0.05)。见表3。
表3 2组患者不同时间MAP、HR、SpO2、VAS评分比较
Table 3 Comparison of MAP, HR, SpO2, and VAS scores between two groups at different time points![]()
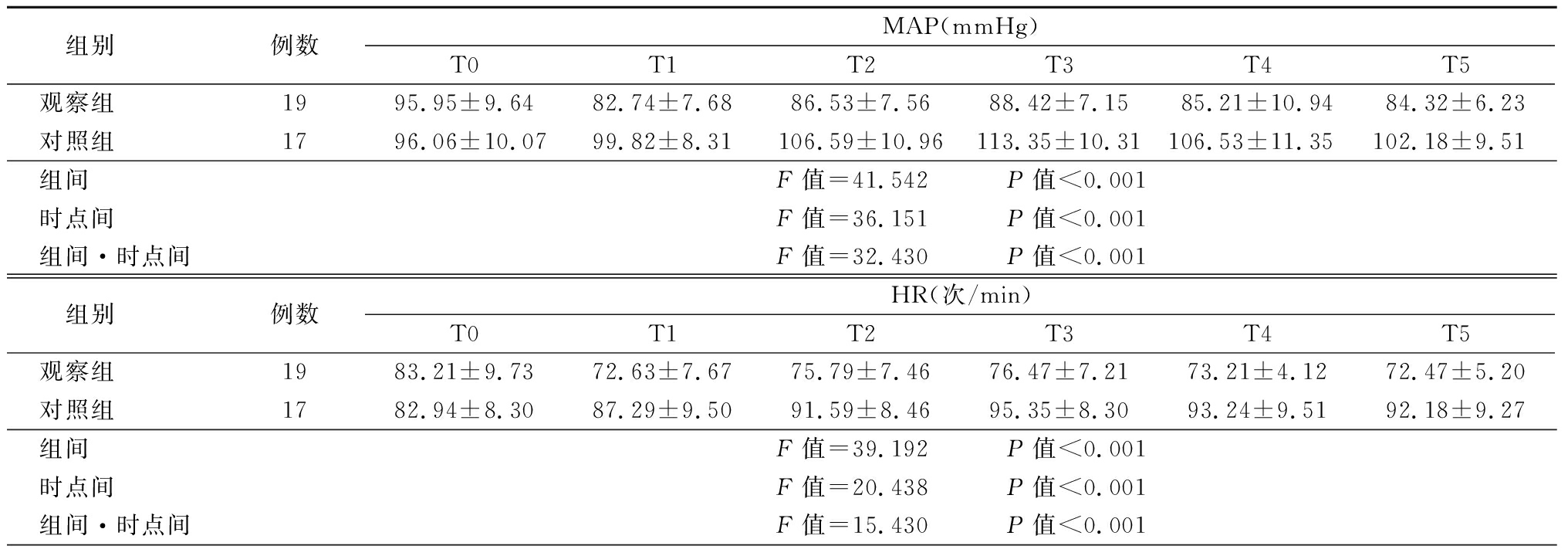
组别 例数MAP(mmHg)T0T1T2T3T4T5观察组 1995.95±9.6482.74±7.6886.53±7.5688.42±7.1585.21±10.9484.32±6.23对照组 1796.06±10.0799.82±8.31106.59±10.96113.35±10.31106.53±11.35102.18±9.51组间 F值=41.542 P值<0.001时点间 F值=36.151 P值<0.001组间·时点间F值=32.430 P值<0.001组别 例数HR(次/min)T0T1T2T3T4T5观察组 1983.21±9.7372.63±7.6775.79±7.4676.47±7.21 73.21±4.1272.47±5.20对照组 1782.94±8.3087.29±9.5091.59±8.4695.35±8.3093.24±9.5192.18±9.27组间 F值=39.192 P值<0.001时点间 F值=20.438 P值<0.001组间·时点间F值=15.430 P值<0.001
表3 (续)
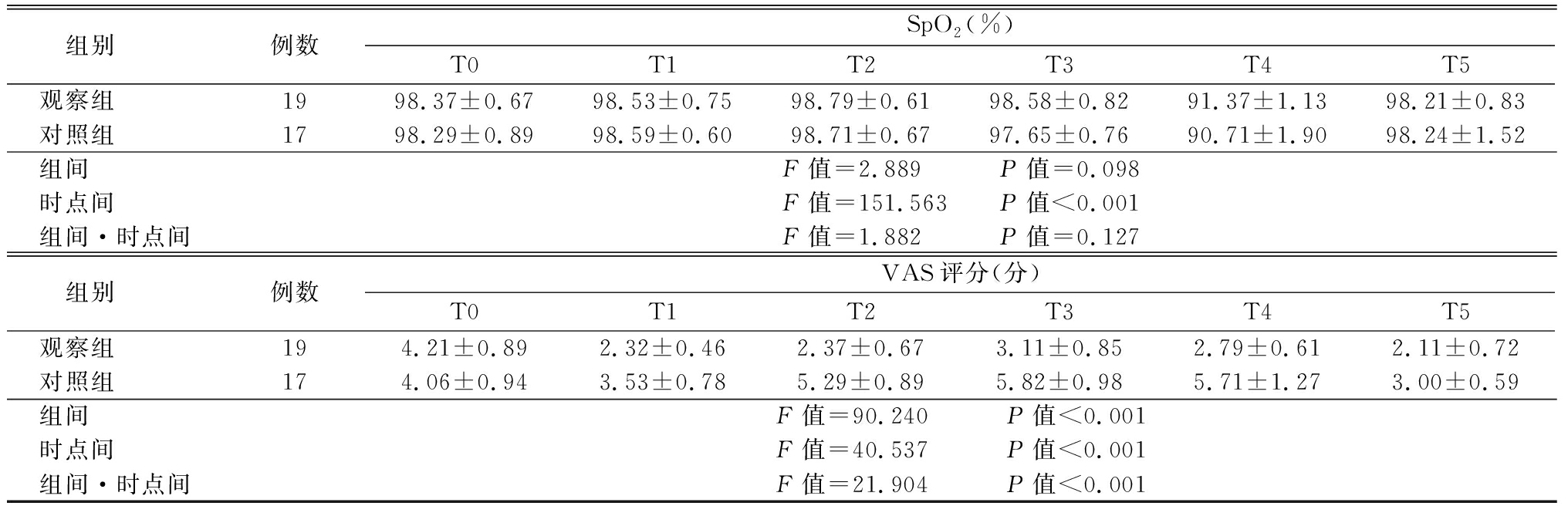
组别 例数SpO2(%)T0T1T2T3T4T5观察组 1998.37±0.6798.53±0.75 98.79±0.6198.58±0.82 91.37±1.1398.21±0.83对照组 1798.29±0.8998.59±0.6098.71±0.6797.65±0.7690.71±1.9098.24±1.52组间 F值=2.889 P值=0.098时点间 F值=151.563 P值<0.001组间·时点间F值=1.882 P值=0.127组别 例数VAS评分(分)T0T1T2T3T4T5观察组 194.21±0.89 2.32±0.462.37±0.673.11±0.852.79±0.612.11±0.72对照组 174.06±0.943.53±0.785.29±0.895.82±0.985.71±1.273.00±0.59组间 F值=90.240 P值<0.001时点间 F值=40.537 P值<0.001组间·时点间F值=21.904 P值<0.001
2.3 2组围手术期麻醉不良反应及并发症发生情况比较 围手术期2组均未发生心动过缓,血氧下降、血压波动等麻醉相关并发症。观察组发生骨水泥渗漏1例,对照组发生骨水泥渗漏2例,但均无临床症状,未予以处理。2组骨水泥渗漏发生率差异无统计学意义(χ2=0.497,P=0.481)。
3 讨 论
老年人由于骨质疏松、身体机能下降及运动能力减退,易在外力、跌倒等意外情况中发生骨折,其中最多见的骨折部位为脊柱骨折,常导致腰背部疼痛、活动受限,甚至脊柱后凸畸形、神经功能障碍等,严重影响生活质量[9]。目前临床主要采用PKP治疗老年骨质疏松性椎体压缩性骨折,具有快速缓解疼痛,允许早期活动的优势[10]。
PKP一般采用局部麻醉,但局部麻醉不能抑制PKP术中球囊扩张及注入骨水泥时产生的剧烈疼痛,而疼痛、紧张等刺激易诱发心脑血管疾病,高龄患者由于全身情况不佳、机体代偿能力差,局部麻醉下手术出现疼痛管理不满意,球囊扩张不充分,血流动力学改变等情况时有发生,导致手术风险增大,影响疗效[11-12]。因此,老年患者需要强化的镇痛方案以降低手术风险。Liu等[4]报道,采用全身麻醉,取得满意麻醉效果,但高龄患者多合并多器官疾病,全身麻醉相关并发症风险较高,术后并发症多发,且全身麻醉操作复杂、费用较高,临床应用受限。基础麻醉是一种手术麻醉前使患者意识消失处于熟睡或前麻醉状态的辅助麻醉方法,常予以静脉给药,达到镇静、抗焦虑、减少应激反应的目的。研究表明,异丙酚、瑞芬太尼等麻醉对脊柱骨折患者疼痛指数和炎症反应具有明显的降低作用,且术后恢复时间短[13]。Mohr等[7]采用米达唑仑和哌腈咪特作为PKP术前基础麻醉,取得满意麻醉效果,且未见麻醉相关并发症发生。Li 等[14]报道,芬太尼联合丙泊酚的清醒麻醉方案用于PKP,虽取得一定疗效,但丙泊酚易致呼吸抑制,特别对于麻醉风险较高的高龄患者,非气管插管下须谨慎使用。右美托咪定是一种高选择性α2肾上腺受体激动剂,具有良好的降低交感神经张力、镇痛、镇静的作用,且对呼吸抑制作用极弱,甚至使用推荐剂量的10倍情况下也能保证安全通气;另外,小计量输注(<1 μg/kg)时可降低血压,控制PKP术中循环系统的波动[14]。尹加林等[12]分析了40例右美托咪定用于局部麻醉PKP术的镇痛效果和对血流动力学影响,证实右美托咪定的清醒镇痛可为PKP提供满意的镇痛效果,降低围手术期血流动力反应。廖兴志等[15]采用随机分组对照的方法,对比不同剂量右美托咪定在PKP术中的应用效果,结果显示,麻醉前10 min以0.7 μg/kg静脉输注有利于维持术中循环稳定,镇静作用良好且不良反应少。对于高龄患者,减少药物负荷剂量以降低不良反应不容忽视,因此,本研究于局部麻醉前10 min以0.5 μg/kg静脉给药,降低负荷剂量,并以0.4 μg·kg-1·h-1维持剂量至手术结束,结果显示,观察组术后疼痛管理满意度评分高于对照组,在围手术期MAP、HR、VAS评分低于对照组,2组围手术期未出现麻醉相关并发症,证实了该强化镇痛方案的安全性和有效性。另外,2组围手术期SpO2组间、时点间、组间·时点间交互作用差异无统计学意义(P>0.05),提示观察组无呼吸抑制等不良反应。
本研究存在几点缺陷:①由于高龄患者药物剂量需减量并个体化用药,需进一步研究来证实最佳负荷剂量;②本研究样本量有限,且为单中心研究,研究方法存在局限,可能存在统计偏差,研究结果需大样本、多中心的对照研究以进一步证实。综上所述,小剂量右美托咪定静脉麻醉联合局部麻醉为高龄PKP患者提供了一种安全、有效的麻醉方法,能有效降低围手术期血流动力反应,值得推广应用。
[1] Yin P,Li Z,Zhu S,et al. The treatment of osteoporotic thoraco-lumbar burst fractures by unilateral percutaneous kyphoplasty: A prospective observation study[J]. Eur J Pain,2020,24(3):659-664.
[2] Liu Z,Zhou Y,Lei F,et al. Effect of percutaneous kyphoplasty with different phases bone cement for treatment of osteoporotic vertebral compression fractures[J]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi,2020,34(4):435-441.
[3] Mccarthy J,Davis A. Diagnosis and management of vertebral compression fractures[J]. Am Fam Physician,2016,94(1):44-50.
[4] Liu J,Wang L,Chai M,et al. Analysis of anesthesia methods in percutaneous kyphoplasty for treatment of vertebral compression fractures[J]. J Healthc Eng,2020,2020: 3965961.
[5] 王爱荣,马云龙.右美托咪定在经皮球囊扩张椎体后凸成形术麻醉中的应用[J].中国医药,2018,13(4):566-569.
[6] 张古月,陆良愿.酮咯酸氨丁三醇联合右美托咪定在老年患者经皮球囊椎体后凸成形术中的应用效果[J].中国当代医药,2019,26(9):105-107.
[7] Mohr M,Pillich D,Kirsch M,et al. Percutaneous balloon kyphoplasty with the patient under intravenous analgesia and sedation: a feasibility study[J]. AJNR Am J Neuroradiol,2011,32(4):649-653.
[8] 张军卫,唐和虎,李想,等. Denis,Magerl和AO2013三种胸腰椎损伤分类方法的对比分析[J].中华骨与关节外科杂志,2017,10(4):312-316.
[9] Kim DH,Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment[J]. Spine J,2006,6(5):479-487.
[10] Wang D,Zheng S,Liu A,et al. The role of minimally invasive vertebral body stent on reduction of the deflation effect after kyphoplasty: a biomechanical study[J]. Spine(Phila Pa 1976),2018,43(6):E341-E347.
[11] 倪跃,龚立,宁仁德,等. PKP结合明胶海绵辅助利多卡因治疗胸腰椎骨折的疗效分析[J].颈腰痛杂志,2019,40(2):170-172.
[12] 尹加林,张勇,吕云落,等.右美托咪定用于老年患者经皮椎体 后凸成形术的镇痛效果[J].临床麻醉学杂志,2013,29(4):353-355.
[13] Zhao Y,Zhang H. Propofol and sevoflurane combined with remifentanil on the pain index,inflammatory factors and postoperative cognitive function of spine fracture patients[J]. Exp Ther Med,2018,15(4):3775-3780.
[14] Li G,Liu H,Wang Q,et al. Preoperative prone position exercises: a simple and novel method to improve tolerance to kyphoplasty for treatment of single level osteoporotic vertebral compression fractures[J]. BMC Musculoskelet Disord,2017,18(1):472.
[15] 廖兴志,刘宇芳,全耀晨,等.右美托咪定在局麻经皮椎体后凸成形术患者的应用[J].江苏医药,2015,41(3):280-282.